
Contributions
Abstract: EP1272
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Salvage chemotherapy followed by high-dose chemotherapy and ASCT is the standard treatment approach for R/R HL patients. This strategy leads to cure of almost half of the patients. Several HL study groups suggest various prognostic factors that identify patients at high risk for failing ASCT. These patients benefit from brentuximab vedotin (BV) consolidation treatment, as suggested by the AETHERA trial.
Aims
The identification of prognostic factors and the construction of an algorithm, to identify individuals at high-risk for progressing after ASCT from a series of consecutive R/R HL patients, treated in a single Unit.
Methods
A total of 189 patients who received ASCT between 1996 and 2020 were retrospectively analysed with a median follow-up of 106 (range 9-369) months, median age: 32 years, 110 males. The following factors were studied: age, sex, histologic type, stage, number of involved fields, extranodal, bulky disease, B-symptoms at diagnosis and at relapse, anemia at relapse (Hb<13 g/dl (males) and <12 g/dl (females), response to 1st line and salvage chemotherapy regimens, number of therapies before ASCT, use of radiotherapy, and disease status pre-transplant as assessed by computed tomography (CT) and positron emission tomography (PET), as well as by a composite score integrating both CT and PET. The primary endpoint was 5-year freedom from progression (FFP). Univariate Kaplan Meier analysis was conducted, followed by multivariate analysis using the Cox Proportional-Hazards Model.
Results
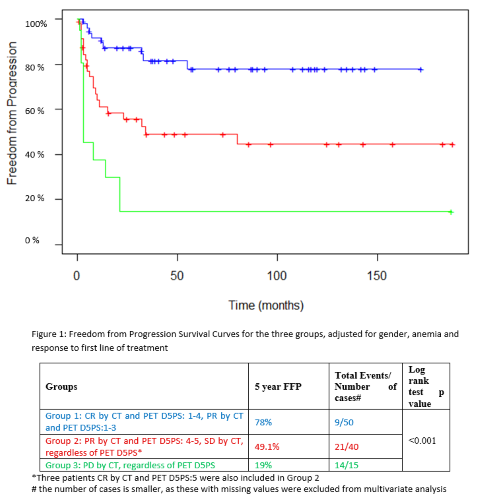
Univariate Analysis revealed the following significant factors for FFP: Response after 1st line and 1st salvage, Early (including primary refractory) vs late relapse, B-symptoms and anemia at relapse, disease status pre-transplant, as assessed by CT, PET and the composite PET and CT score. The latter was the factor with the highest significance (p<0.001), that could stratify patients into three groups with different outcomes. The 1st group included patients with complete remission (CR) by CT and PET up to Deauville 5-point scale (D5PS) of 4, and those with partial remission (PR) by CT and PET D5PS 1-3; the 2nd group included patients in PR by CT and PET D5PS 4-5, and those with stable disease (SD) by CT regardless of PET; finally the 3rd group included patients with progressive disease (PD) by CT, regardless of PET.
By multivariate Cox Regression analysis 2 factors remained significant: 1. The composite PET and CT score pre-transplant showed that patients of group 2 and 3 are more likely to relapse after ASCT, compared to those of group 1, ( p=0.002, <0.001, hazard ratio 3.45 and 9.49, respectively), 2. Anemia at relapse; patients presenting without anemia at relapse had 51% less risk of progression (p= 0.033). PD and PR after 1st line of treatment show almost double, but marginally significant (p= 0.046 and 0.055, respectively) risk for progression, and SD was insignificant( p=0.99), but few cases were included (N=8).
Conclusion
Analysis of real world data showed that disease status assessment using both CT and PET prior to transplant can direct therapeutic strategy in R/R HL patients undergoing ASCT. Patients with PD do not benefit from the procedure and should be treated with alternative treatment. Patients with CR by CT and PET up to D5PS of 4 or these with PR by CT and PET up to D5PS 3, show excellent prognosis and do not need consolidation treatment post ASCT. The remaining ones representing 25% of the population are those who may benefit from BV maintenance. This strategy is currently adopted by our center.
Keyword(s): Autologous hematopoietic stem cell transplantation, Consolidation, Hodgkin's lymphoma, Prognostic factor
Abstract: EP1272
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Salvage chemotherapy followed by high-dose chemotherapy and ASCT is the standard treatment approach for R/R HL patients. This strategy leads to cure of almost half of the patients. Several HL study groups suggest various prognostic factors that identify patients at high risk for failing ASCT. These patients benefit from brentuximab vedotin (BV) consolidation treatment, as suggested by the AETHERA trial.
Aims
The identification of prognostic factors and the construction of an algorithm, to identify individuals at high-risk for progressing after ASCT from a series of consecutive R/R HL patients, treated in a single Unit.
Methods
A total of 189 patients who received ASCT between 1996 and 2020 were retrospectively analysed with a median follow-up of 106 (range 9-369) months, median age: 32 years, 110 males. The following factors were studied: age, sex, histologic type, stage, number of involved fields, extranodal, bulky disease, B-symptoms at diagnosis and at relapse, anemia at relapse (Hb<13 g/dl (males) and <12 g/dl (females), response to 1st line and salvage chemotherapy regimens, number of therapies before ASCT, use of radiotherapy, and disease status pre-transplant as assessed by computed tomography (CT) and positron emission tomography (PET), as well as by a composite score integrating both CT and PET. The primary endpoint was 5-year freedom from progression (FFP). Univariate Kaplan Meier analysis was conducted, followed by multivariate analysis using the Cox Proportional-Hazards Model.
Results
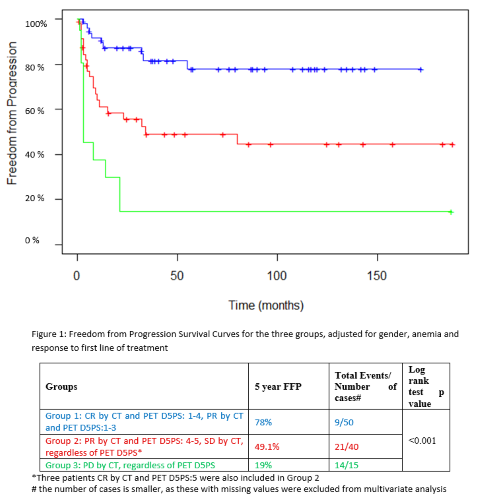
Univariate Analysis revealed the following significant factors for FFP: Response after 1st line and 1st salvage, Early (including primary refractory) vs late relapse, B-symptoms and anemia at relapse, disease status pre-transplant, as assessed by CT, PET and the composite PET and CT score. The latter was the factor with the highest significance (p<0.001), that could stratify patients into three groups with different outcomes. The 1st group included patients with complete remission (CR) by CT and PET up to Deauville 5-point scale (D5PS) of 4, and those with partial remission (PR) by CT and PET D5PS 1-3; the 2nd group included patients in PR by CT and PET D5PS 4-5, and those with stable disease (SD) by CT regardless of PET; finally the 3rd group included patients with progressive disease (PD) by CT, regardless of PET.
By multivariate Cox Regression analysis 2 factors remained significant: 1. The composite PET and CT score pre-transplant showed that patients of group 2 and 3 are more likely to relapse after ASCT, compared to those of group 1, ( p=0.002, <0.001, hazard ratio 3.45 and 9.49, respectively), 2. Anemia at relapse; patients presenting without anemia at relapse had 51% less risk of progression (p= 0.033). PD and PR after 1st line of treatment show almost double, but marginally significant (p= 0.046 and 0.055, respectively) risk for progression, and SD was insignificant( p=0.99), but few cases were included (N=8).
Conclusion
Analysis of real world data showed that disease status assessment using both CT and PET prior to transplant can direct therapeutic strategy in R/R HL patients undergoing ASCT. Patients with PD do not benefit from the procedure and should be treated with alternative treatment. Patients with CR by CT and PET up to D5PS of 4 or these with PR by CT and PET up to D5PS 3, show excellent prognosis and do not need consolidation treatment post ASCT. The remaining ones representing 25% of the population are those who may benefit from BV maintenance. This strategy is currently adopted by our center.
Keyword(s): Autologous hematopoietic stem cell transplantation, Consolidation, Hodgkin's lymphoma, Prognostic factor


