
Contributions
Abstract: EP1263
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
CMV reactivation continues to be a significant clinical problem after allogeneic stem cell transplantation (allo-HSCT). CMV (IgG) seropositivity before allo-HSCT is an important risk factor for CMV reactivation and CMV disease. Without prophylaxis, CMV infections occur in approximately 60-80% patients after allo-HSCT, usually in the early post-transplant period. Any level of CMV viremia is associated with increased non-relapse mortality in the first year post allo-HSCT. In 2019 at UHC Zagreb the preemptive CMV treatment approach was substituted with letermovir prophylaxis
Aims
The aim of this study was to analyse the population of patients who received letermovir, and to compare them with historical controls.
Methods
We retrospectively analysed 90 consecutive patients who underwent allo-HSCT between mid-2019 and mid-2020 in our Center.
Results
Median age of patients was 52.5 years, 49% of them were female and only 8.9% CMV seronegative. The most frequent indication for transplantation was acute leukaemia (53%) with peripheral blood stem cells (88%) from unrelated donor (62%) being the most common source of stem cells. Conditioning was of reduced intensity in most of the cases (86%). The patients received letermovir prophylaxis starting from a median of 18.5 days (range 5-28) after allo-HSCT during 90 or until CMV reactivation. With a median follow-up of 385 days (range 152-636), 26 patients (29%) experienced CMV breakthrough while on letermovir, 12 within 100 days, and 14 after day 100 post allo-HSCT. In 22 patients preemptive treatment was started and two patients developed CMV disease (pneumonitis). In one patient muscle and joint pain occurred, possibly related to letermovir, no other adverse events were noticed.
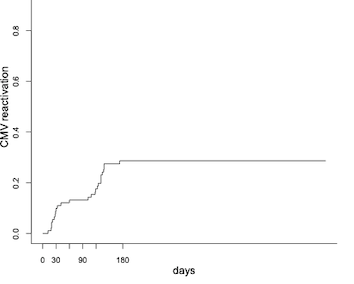
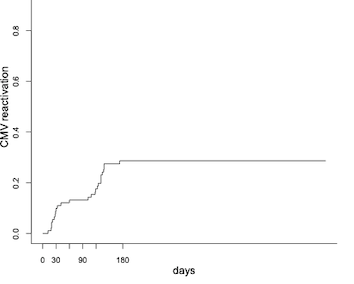
Cumulative incidence of CMV reactivation at day 180 was lower in letermovir group: 29% (95% CI 20-38; median 105 days, range 12-173) compared to historical group (with similar demographic characteristics): 61% (95% CI 53-68; median 27 days, range 1-131). Patients with detectable virus level <137 IU/ml were also started on letermovir prophylaxis, and were found to have higher cumulative incidence of CMV reactivation 53% (95% CI 26-7), compared to patients who were CMV DNA negative 23% (95% CI 14-33), p=0.002. At day 500 overall survival was 76% (95% CI 65-88) in patients without CMV reactivation compared to 75% (95%CI 53-100) with CMV reactivation.
Conclusion
Our “real-world” experience confirms the efficacy of letermovir in CMV prophylaxis, its favourable safety profile and lack of negative impact on engraftment. We showed a striking decrease in the incidence of CMV reactivation in patients on letermovir prophylaxis compared to similar patient cohort from the same institution during the “preemptive treatment” era, justifying the prophylactic approach. Given the connection between CMV reactivation and NRM, clinicians should be encouraged to use different anti-CMV options available to prevent or at least delay CMV reactivation and CMV disease in transplanted patients. Patients with low, but detectable CMV levels (<137 IU/mL) and patients with the highest risk of CMV reactivation (such as patients with GvHD receiving corticosteroids, or patients who received ATG) might need a specifically tailored anti-CMV approach. Further studies addressing these questions are warranted.
Keyword(s): CMV infection, Stem cell transplant
Abstract: EP1263
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
CMV reactivation continues to be a significant clinical problem after allogeneic stem cell transplantation (allo-HSCT). CMV (IgG) seropositivity before allo-HSCT is an important risk factor for CMV reactivation and CMV disease. Without prophylaxis, CMV infections occur in approximately 60-80% patients after allo-HSCT, usually in the early post-transplant period. Any level of CMV viremia is associated with increased non-relapse mortality in the first year post allo-HSCT. In 2019 at UHC Zagreb the preemptive CMV treatment approach was substituted with letermovir prophylaxis
Aims
The aim of this study was to analyse the population of patients who received letermovir, and to compare them with historical controls.
Methods
We retrospectively analysed 90 consecutive patients who underwent allo-HSCT between mid-2019 and mid-2020 in our Center.
Results
Median age of patients was 52.5 years, 49% of them were female and only 8.9% CMV seronegative. The most frequent indication for transplantation was acute leukaemia (53%) with peripheral blood stem cells (88%) from unrelated donor (62%) being the most common source of stem cells. Conditioning was of reduced intensity in most of the cases (86%). The patients received letermovir prophylaxis starting from a median of 18.5 days (range 5-28) after allo-HSCT during 90 or until CMV reactivation. With a median follow-up of 385 days (range 152-636), 26 patients (29%) experienced CMV breakthrough while on letermovir, 12 within 100 days, and 14 after day 100 post allo-HSCT. In 22 patients preemptive treatment was started and two patients developed CMV disease (pneumonitis). In one patient muscle and joint pain occurred, possibly related to letermovir, no other adverse events were noticed.
Cumulative incidence of CMV reactivation at day 180 was lower in letermovir group: 29% (95% CI 20-38; median 105 days, range 12-173) compared to historical group (with similar demographic characteristics): 61% (95% CI 53-68; median 27 days, range 1-131). Patients with detectable virus level <137 IU/ml were also started on letermovir prophylaxis, and were found to have higher cumulative incidence of CMV reactivation 53% (95% CI 26-7), compared to patients who were CMV DNA negative 23% (95% CI 14-33), p=0.002. At day 500 overall survival was 76% (95% CI 65-88) in patients without CMV reactivation compared to 75% (95%CI 53-100) with CMV reactivation.
Conclusion
Our “real-world” experience confirms the efficacy of letermovir in CMV prophylaxis, its favourable safety profile and lack of negative impact on engraftment. We showed a striking decrease in the incidence of CMV reactivation in patients on letermovir prophylaxis compared to similar patient cohort from the same institution during the “preemptive treatment” era, justifying the prophylactic approach. Given the connection between CMV reactivation and NRM, clinicians should be encouraged to use different anti-CMV options available to prevent or at least delay CMV reactivation and CMV disease in transplanted patients. Patients with low, but detectable CMV levels (<137 IU/mL) and patients with the highest risk of CMV reactivation (such as patients with GvHD receiving corticosteroids, or patients who received ATG) might need a specifically tailored anti-CMV approach. Further studies addressing these questions are warranted.
Keyword(s): CMV infection, Stem cell transplant


