
Contributions
Abstract: EP1262
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Historically, sequential transplant regimen using fludarabine/cytosine arabinoside/amsacrine (FLAMSA) cytoreduction followed by busulfan (Bu) based regimen has been associated with improved outcome in high-risk myeloid neoplasms (Schmid et al. J Clin Oncol 2005). Recently, Craddock et al. showed prospectively that FLAMSA-RIC was not associated with survival benefit compared to classical reduced intensity conditioning (RIC) regimens, especially in patients who experienced positive minimal residual disease (MRD) prior hematopoietic stem cell transplantation (HSCT)(Craddock et al. Blood 2020).
Aims
In this monocentric study, we aimed to evaluate retrospectively the outcome of patients receiving FLAMSA-Bu based conditioning regimens for high-risk myeloid neoplasms.
Methods
We analyzed 203 patients who received FLAMSA-Bu based conditioning regiments for high-risk AML (N=165), myelodysplastic syndrome (MDS)(N=32) or MDS/myeloproliferative neoplasms (MPN) (N=6), between October 2011 and June 2020. In AML setting, flow cytometry minimal residual disease (MRD) was available in 151/165 patient prior transplant and based on leukemia associated immunophenotype (LAIP) using ELN recommendations (bulk lyses, and at least 500 000 live cells to achieve a sensitivity of 0.1%). MRD flow was performed in bone marrow samples using 8 color panel.
Results
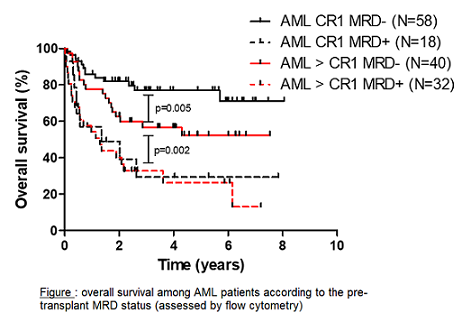
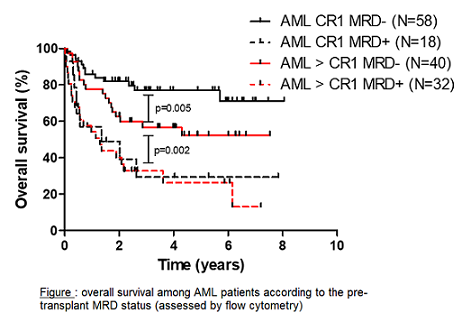
The median follow-up post HSCT time was 32,2 months (0.0—98 months). At 3 years, overall survival (OS) was 56% and 39.8% in AML and MDS settings respectively. In the AML cohort, ELN 2013 classification was not predictive for survival or cumulative incidence of relapse (CIR). When available, results were similar regarding ELN 2017 classification. For patients in CR1 (1st complete remission) at the time of HSCT, median OS was not reached. For those in > CR1 or refractory at the time of HSCT, median OS was 34.3 and 25.6 months respectively (p=0.56). For AML patients in CR1, pre-HSCT MRD+ (defined positive when ≥ 0.1%) was highly predictive for relapse, which reached 57.3% at 3 years. For pre-HSCT MRD- patients, median OS was not reached either patients where in CR1 or more. However, median OS was not statistically different for pre-HSCT MRD+ patients whatever was the pre-HSCT CR status (refractory excluded) (figure). Finally, MRD- patients receiving myeloablative (Bu4) regimen (MAC) has superior outcome compared to RIC (Bu2). However, neither MAC or RIC abrogated negative impact of pre-HSCT MRD positivity. Post-transplant, neither acute GVHD, chronic GVHD, prophylactic donor lymphocyte infusion or partial chimerism (at day+30, +60 or +90) were associated with survival. Regarding donor type, TRM was 14,1%, 29% and 37.3%, whereas cytologic relapse occurred in 32%, 20.3% and 15.1% cases in HLA-identical, matched-unrelated (MUD) and mismatched unrelated donor (MMUD) respectively. TRM was significantly higher in patients aged over 55 years old (38%) compared to younger ones (age < 45 = 14.9%, age 46-55 = 22%) (p=0.03). In multivariate analysis, only prior HSCT MRD status and age remained of statistical significance regarding survival in AML patients.
Conclusion
Our results emphasize that FLAMSA conditioning regimen is an interesting strategy in high-risk myeloid neoplasm, even in refractory AML patients. Despite abrogating the impact of ELN risk groups in AML settings, pre-HSCT MRD status remains the main detrimental factor for relapse probability. Moreover, advanced age was associated with high rate of TRM suggesting that such strategy should be avoided, especially in adults aged over 55 years old.
Keyword(s): AML, Conditioning, HSCT, MRD
Abstract: EP1262
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Historically, sequential transplant regimen using fludarabine/cytosine arabinoside/amsacrine (FLAMSA) cytoreduction followed by busulfan (Bu) based regimen has been associated with improved outcome in high-risk myeloid neoplasms (Schmid et al. J Clin Oncol 2005). Recently, Craddock et al. showed prospectively that FLAMSA-RIC was not associated with survival benefit compared to classical reduced intensity conditioning (RIC) regimens, especially in patients who experienced positive minimal residual disease (MRD) prior hematopoietic stem cell transplantation (HSCT)(Craddock et al. Blood 2020).
Aims
In this monocentric study, we aimed to evaluate retrospectively the outcome of patients receiving FLAMSA-Bu based conditioning regimens for high-risk myeloid neoplasms.
Methods
We analyzed 203 patients who received FLAMSA-Bu based conditioning regiments for high-risk AML (N=165), myelodysplastic syndrome (MDS)(N=32) or MDS/myeloproliferative neoplasms (MPN) (N=6), between October 2011 and June 2020. In AML setting, flow cytometry minimal residual disease (MRD) was available in 151/165 patient prior transplant and based on leukemia associated immunophenotype (LAIP) using ELN recommendations (bulk lyses, and at least 500 000 live cells to achieve a sensitivity of 0.1%). MRD flow was performed in bone marrow samples using 8 color panel.
Results
The median follow-up post HSCT time was 32,2 months (0.0—98 months). At 3 years, overall survival (OS) was 56% and 39.8% in AML and MDS settings respectively. In the AML cohort, ELN 2013 classification was not predictive for survival or cumulative incidence of relapse (CIR). When available, results were similar regarding ELN 2017 classification. For patients in CR1 (1st complete remission) at the time of HSCT, median OS was not reached. For those in > CR1 or refractory at the time of HSCT, median OS was 34.3 and 25.6 months respectively (p=0.56). For AML patients in CR1, pre-HSCT MRD+ (defined positive when ≥ 0.1%) was highly predictive for relapse, which reached 57.3% at 3 years. For pre-HSCT MRD- patients, median OS was not reached either patients where in CR1 or more. However, median OS was not statistically different for pre-HSCT MRD+ patients whatever was the pre-HSCT CR status (refractory excluded) (figure). Finally, MRD- patients receiving myeloablative (Bu4) regimen (MAC) has superior outcome compared to RIC (Bu2). However, neither MAC or RIC abrogated negative impact of pre-HSCT MRD positivity. Post-transplant, neither acute GVHD, chronic GVHD, prophylactic donor lymphocyte infusion or partial chimerism (at day+30, +60 or +90) were associated with survival. Regarding donor type, TRM was 14,1%, 29% and 37.3%, whereas cytologic relapse occurred in 32%, 20.3% and 15.1% cases in HLA-identical, matched-unrelated (MUD) and mismatched unrelated donor (MMUD) respectively. TRM was significantly higher in patients aged over 55 years old (38%) compared to younger ones (age < 45 = 14.9%, age 46-55 = 22%) (p=0.03). In multivariate analysis, only prior HSCT MRD status and age remained of statistical significance regarding survival in AML patients.
Conclusion
Our results emphasize that FLAMSA conditioning regimen is an interesting strategy in high-risk myeloid neoplasm, even in refractory AML patients. Despite abrogating the impact of ELN risk groups in AML settings, pre-HSCT MRD status remains the main detrimental factor for relapse probability. Moreover, advanced age was associated with high rate of TRM suggesting that such strategy should be avoided, especially in adults aged over 55 years old.
Keyword(s): AML, Conditioning, HSCT, MRD


