
Contributions
Abstract: EP1261
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Evidence is emerging to support an association between certain HLA alleles, and the risk of CMV reactivation post-allo-HSCT. HLA alleles associated with resistance to CMV reactivation have been referred to as “CMV immunodominant alleles”, and are thought to present viral antigen to T lymphocytes more effectively.
Aims
We aimed to identify HLA alleles associated with either resistance or susceptibility to CMV reactivation.
Methods
We studied 586 adults who underwent allo-HSCT. We included patients who had engrafted successfully, and had been typed at HLA-A, B, C, DRB1 and DQB1 loci by next-generation sequencing. Weekly CMV monitoring by PCR was done on whole blood, and anti-viral treatment was initiated for levels more than 200 IU/ml.
The primary outcome measure was the occurrence of CMV reactivation needing treatment, with or without CMV disease. Hazard ratios were calculated by Cox regression analyses, for HLA alleles and other variables significantly associated with CMV reactivation. We analysed only HLA Class I and II alleles that were observed at a frequency of >5% in donor or recipient cohorts, and adjusted for the effect of multiple comparisons.
Results
The median patient age was 57 years. AML was the most common diagnosis (51.5% patients). Donor types were as follows: matched unrelated (MUD; 52.5%); matched related (19%); mismatched unrelated (MMUD; 18%); and haploidentical (11%) donors. Eighty nine percent received a T-cell depleting agent during conditioning.
The cumulative incidence of CMV reactivation in the entire cohort at 6 months was 55% (95%CI 51%>59%).
This was significantly higher in recipients of MMUD and haploidentical grafts, and in those with a pre-transplant CMV IgG serostatus either donor positive/recipient positive or donor negative/recipient positive.
The one-year overall survival in patients with and without CMV reactivation were 54% and 63%
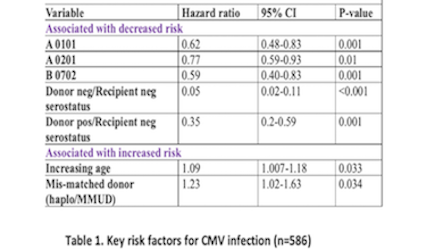
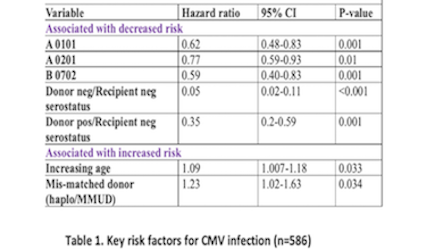
respectively (p=0.01). The univariate analysis indicated that alleles HLA A*01:01 (HR 0.62, 95% CI 0.48-0.83), A*02:01 (HR-0.77, 95% CI 0.59-0.93), and B*07:02 (HR 0.59, 95% CI 0.40-0.83) were associated with protection against CMV (Table 1). Other factors impacting risk of CMV reactivation on univariate analysis were increasing recipient age, use of T-cell depletion, mismatched donor (haploidentical or MMUD), and pre-transplant CMV serostatus. These factors, along with the significantly associated HLA alleles were included in a multivariable model. Mismatched donor (HR 1.23, 95% CI 1.02-1.63) and increasing age (HR 1.09, 95% CI 1.007-1.18) were independently associated with increased risk of CMV reactivation, whereas donor negative/recipient negative
serostatus (HR 0.05, 95% CI 0.02-0.11), donor positive/recipient negative serostatus (HR 0.35, 95% CI 0.20-0.59), and HLA B*07:02 (HR 0.63, 95% CI 0.44-0.88) were independently associated with protection against CMV reactivation.
Patients who developed CMV reactivation had lower overall survival (HR 0.62, 95% CI 0.46-0.82), higher transplant related mortality (TRM; HR 1.72, 95% CI 1.25-2.36), lower relapse (HR 0.58, 95% CI 0.41-0.82) and similar relapse free survival (RFS) when compared to those who did not develop CMV reactivation. The number of CMV reactivations had no effect on TRM.
Conclusion
HLA B*07:02 was associated with protection against CMV reactivation post-transplant. Although CMV reactivation was associated with increased TRM, it was also associated with decreased relapse rates, resulting in similar RFS post-transplant compared to patients not developing CMV reactivation.
Keyword(s): Allogeneic hematopoietic stem cell transplant, Cytomegalovirus, HLA
Abstract: EP1261
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Evidence is emerging to support an association between certain HLA alleles, and the risk of CMV reactivation post-allo-HSCT. HLA alleles associated with resistance to CMV reactivation have been referred to as “CMV immunodominant alleles”, and are thought to present viral antigen to T lymphocytes more effectively.
Aims
We aimed to identify HLA alleles associated with either resistance or susceptibility to CMV reactivation.
Methods
We studied 586 adults who underwent allo-HSCT. We included patients who had engrafted successfully, and had been typed at HLA-A, B, C, DRB1 and DQB1 loci by next-generation sequencing. Weekly CMV monitoring by PCR was done on whole blood, and anti-viral treatment was initiated for levels more than 200 IU/ml.
The primary outcome measure was the occurrence of CMV reactivation needing treatment, with or without CMV disease. Hazard ratios were calculated by Cox regression analyses, for HLA alleles and other variables significantly associated with CMV reactivation. We analysed only HLA Class I and II alleles that were observed at a frequency of >5% in donor or recipient cohorts, and adjusted for the effect of multiple comparisons.
Results
The median patient age was 57 years. AML was the most common diagnosis (51.5% patients). Donor types were as follows: matched unrelated (MUD; 52.5%); matched related (19%); mismatched unrelated (MMUD; 18%); and haploidentical (11%) donors. Eighty nine percent received a T-cell depleting agent during conditioning.
The cumulative incidence of CMV reactivation in the entire cohort at 6 months was 55% (95%CI 51%>59%).
This was significantly higher in recipients of MMUD and haploidentical grafts, and in those with a pre-transplant CMV IgG serostatus either donor positive/recipient positive or donor negative/recipient positive.
The one-year overall survival in patients with and without CMV reactivation were 54% and 63%
respectively (p=0.01). The univariate analysis indicated that alleles HLA A*01:01 (HR 0.62, 95% CI 0.48-0.83), A*02:01 (HR-0.77, 95% CI 0.59-0.93), and B*07:02 (HR 0.59, 95% CI 0.40-0.83) were associated with protection against CMV (Table 1). Other factors impacting risk of CMV reactivation on univariate analysis were increasing recipient age, use of T-cell depletion, mismatched donor (haploidentical or MMUD), and pre-transplant CMV serostatus. These factors, along with the significantly associated HLA alleles were included in a multivariable model. Mismatched donor (HR 1.23, 95% CI 1.02-1.63) and increasing age (HR 1.09, 95% CI 1.007-1.18) were independently associated with increased risk of CMV reactivation, whereas donor negative/recipient negative
serostatus (HR 0.05, 95% CI 0.02-0.11), donor positive/recipient negative serostatus (HR 0.35, 95% CI 0.20-0.59), and HLA B*07:02 (HR 0.63, 95% CI 0.44-0.88) were independently associated with protection against CMV reactivation.
Patients who developed CMV reactivation had lower overall survival (HR 0.62, 95% CI 0.46-0.82), higher transplant related mortality (TRM; HR 1.72, 95% CI 1.25-2.36), lower relapse (HR 0.58, 95% CI 0.41-0.82) and similar relapse free survival (RFS) when compared to those who did not develop CMV reactivation. The number of CMV reactivations had no effect on TRM.
Conclusion
HLA B*07:02 was associated with protection against CMV reactivation post-transplant. Although CMV reactivation was associated with increased TRM, it was also associated with decreased relapse rates, resulting in similar RFS post-transplant compared to patients not developing CMV reactivation.
Keyword(s): Allogeneic hematopoietic stem cell transplant, Cytomegalovirus, HLA


