
Contributions
Abstract: EP1260
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is a curative option for high-risk acute leukemias. But one of the main causes of treatment failure after allo-HSCT for acute leukemia (AL) is still the disease relapse. Currently, minimal residual disease (MRD), detected by multiparameter flow cytometry (MPC), is widely used to identify patients at high risk of relapse due to its availability and the ability to obtain results in a short time frame.
Aims
To assess the predictive value of pre-transplant MRD status.
Methods
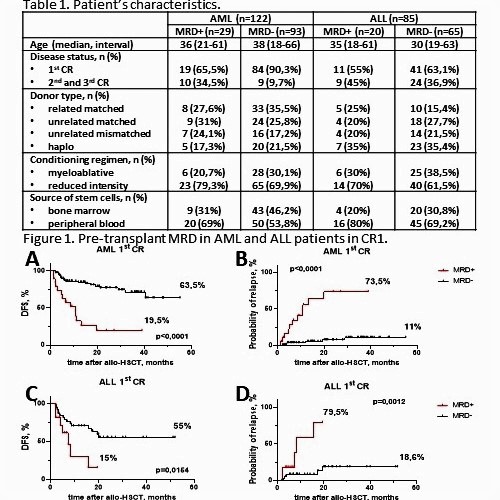
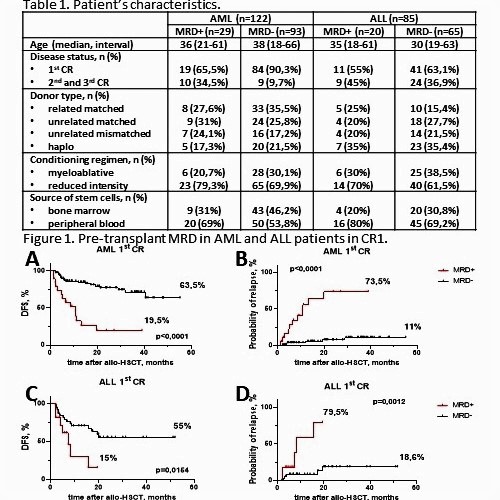
We included 207 patients: 122 patients AML and 85 patients with ALL, who underwent allo-HSCT National Research Center for Hematology between September 2015 and December 2020. Patient characteristics are summarized in Table 1. All patients were in complete morphological remission (CR) at the time of allo-HSCT. The median follow-up was 17 (1,5-55) months for AML and 11,7 (1-64) months for ALL. 6-color MFC was performed on bone marrow samples obtained before allo-HSCT. MRD was detected using a combination of the “different-from-normal” and LAIP methods. The probabilities of DFS and relapse were estimated using the Kaplan–Meier method for all patients. The value of p < 0.05 was considered as significant. Statistical analysis was performed using SPSS ver. 23 (IBM, Chicago, Ill., USA). Cox proportional hazards model was used to assess the influence of various independent factors on the probability of relapse/death from any cause. The factors included in the model: disease status, donor type, conditioning regimen, source of graft, pre-transplant MRD status, age, acute or chronic graft versus host disease (GVHD).
Results
In univariate analysis, the DFS of MRD+ patients with AL in the 1st CR was significantly worse than MRD- (AML: 19,5% vs 63,5%, p <0.0001 (Fig.1A), ALL: 15% vs 55%, p = 0.0154(Fig.1C)), and the probability of relapse in MRD+ patients was significantly higher (AML: 73,5% vs 11%, p <0,0001 (Fig.1B), ALL: 79,5% vs 18,6%, p = 0,0012 (Fig.1C)). Pre-transplant MRD status was not prognostically significant for AL-patients in the 2nd and 3rd remission. In our study, the presence of MRD before allo-HSCT has been shown to be an independent factor influencing the probability of relapse/death (HR = 3,673 [2,185- 6,174], p<0,0001). In turn, it was noted that the development of chronic GVHD reduces post-transplant mortality if it does not require systemic therapy with glucocorticosteroides (HR = 0,183 [0,065-0,516], p=0,001).
Conclusion
Pre-transplant MRD is an independent factor of a poor prognosis. Testing for MRD before allo-HSCT is extremely important to stratify the risk of allo-HSCT and identify patients with AML or ALL who need early interventions such as withdrawal of immune suppression, donor lymphocyte infusion or preemptive chemotherapy in order to prevent the disease relapse.
Keyword(s): Acute leukemia, Allogeneic stem cell transplant, Minimal residual disease (MRD)
Abstract: EP1260
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is a curative option for high-risk acute leukemias. But one of the main causes of treatment failure after allo-HSCT for acute leukemia (AL) is still the disease relapse. Currently, minimal residual disease (MRD), detected by multiparameter flow cytometry (MPC), is widely used to identify patients at high risk of relapse due to its availability and the ability to obtain results in a short time frame.
Aims
To assess the predictive value of pre-transplant MRD status.
Methods
We included 207 patients: 122 patients AML and 85 patients with ALL, who underwent allo-HSCT National Research Center for Hematology between September 2015 and December 2020. Patient characteristics are summarized in Table 1. All patients were in complete morphological remission (CR) at the time of allo-HSCT. The median follow-up was 17 (1,5-55) months for AML and 11,7 (1-64) months for ALL. 6-color MFC was performed on bone marrow samples obtained before allo-HSCT. MRD was detected using a combination of the “different-from-normal” and LAIP methods. The probabilities of DFS and relapse were estimated using the Kaplan–Meier method for all patients. The value of p < 0.05 was considered as significant. Statistical analysis was performed using SPSS ver. 23 (IBM, Chicago, Ill., USA). Cox proportional hazards model was used to assess the influence of various independent factors on the probability of relapse/death from any cause. The factors included in the model: disease status, donor type, conditioning regimen, source of graft, pre-transplant MRD status, age, acute or chronic graft versus host disease (GVHD).
Results
In univariate analysis, the DFS of MRD+ patients with AL in the 1st CR was significantly worse than MRD- (AML: 19,5% vs 63,5%, p <0.0001 (Fig.1A), ALL: 15% vs 55%, p = 0.0154(Fig.1C)), and the probability of relapse in MRD+ patients was significantly higher (AML: 73,5% vs 11%, p <0,0001 (Fig.1B), ALL: 79,5% vs 18,6%, p = 0,0012 (Fig.1C)). Pre-transplant MRD status was not prognostically significant for AL-patients in the 2nd and 3rd remission. In our study, the presence of MRD before allo-HSCT has been shown to be an independent factor influencing the probability of relapse/death (HR = 3,673 [2,185- 6,174], p<0,0001). In turn, it was noted that the development of chronic GVHD reduces post-transplant mortality if it does not require systemic therapy with glucocorticosteroides (HR = 0,183 [0,065-0,516], p=0,001).
Conclusion
Pre-transplant MRD is an independent factor of a poor prognosis. Testing for MRD before allo-HSCT is extremely important to stratify the risk of allo-HSCT and identify patients with AML or ALL who need early interventions such as withdrawal of immune suppression, donor lymphocyte infusion or preemptive chemotherapy in order to prevent the disease relapse.
Keyword(s): Acute leukemia, Allogeneic stem cell transplant, Minimal residual disease (MRD)


