
Contributions
Abstract: EP1253
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Allogeneic hematopoietic stem cell transplantation (AHSCT) is a curative option in hematological malignancies. However, relapse is the first cause of transplant failure. Risk of relapse depends on disease and transplant characteristics 1-4.
The best approach after relapse hasn´t been defined and as prognosis is so poor, AHSCT2 is considered for some patients mainly if relapse after 6 months and are fit enough. Many questions remain regarding the best strategy for AHSCT2.
Aims
The aim of this study was to analyze our center´s experience in patients receiving AHSCT2 in order to identify possible factors to improve management and OS in these patients.
Methods
From 1995, 1119 patients have received an AHSCT in our Unit. Of them, 53 (4.7%) received AHSCT2. A retrospective analysis of data included in our Transplant data base was performed. Statistical analysis was performed with SPSS.
Results
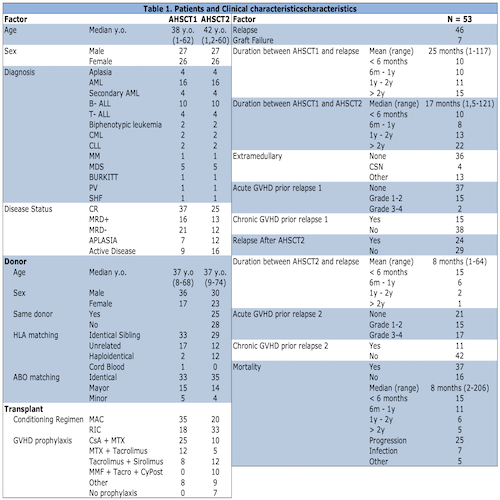
Patients’ characteristics are summarized in Table 1. Median age at AHSCT2 was 35 years old (range 1 to 65). Mean time between AHSCT1 and relapse was 25 months (range 1 to 117) and median time between AHSCTs was 17 months (range 1.5 to 121) Cause of AHSCT2 was relapse for 46/53 (87%) patients and graft failure for 7/53 (13%), of this latter 6/7 (86%) are still alive with graft recovery.
Most frequent diagnosis was primary acute leukemia (57%) (AML= 30%, B- ALL= 20% and T- ALL= 7%). Disease status at AHSCT2 was CR 25/53 (47%) (12/25 (48%) MRD negative), aplasia 12/53 (23%) and active disease (AD) in 16/53 (30%) respectively. Conditioning regimen was Myeloablative (MAC) in 35/53 (66%) for AHSCT 1 and in 20/53 (38%) of the patients for AHSCT2.
Donor was the same in 25/53 (47%) of the transplants. Donor was HLA identical sibling in 29/53 (55%), unrelated in 12/53 (23%) and haploidentical in 12/53 (23%) respectively.
With a median follow-up of 11 months (range 2 to 253) and 54 months (range 3 to 253) for surviving patients, 37 patients have died and 16 (30%) are still alive, 15/16 (94%) disease free. 12/37 patients die due to causes different from progression with Non relapse mortality of 32%.
The 2- and 4-years OS was 39% (SD ± 0.070) and 34% (SD ± 0.069) and the 2- and 4- years PFS was 35% (SD ± 0.067) and 33% (SD ± 0.066) respectively.
Thirty- two (60%) patients presented acute GVHD (aGVHD), 97% involving skin and/or gut. 11/53 (21%) presented Chronic GVDH after AHSCT2.
In the multivariate analysis, the variables which influenced OS were CR vs AD at AHSCT2 (HR 7.96, 95% CI: 2.67–23.78, p <0.001), MAC vs RIC (HR 7.79, 95% CI: 2.55–23.85, p <0.001) and relapse <25 months vs >25 months after AHSCT1 (HR 18.16, 95% CI: 2.03–162.178, p=0.009). HLA matching had no statistically significant impact on OS Identical sibling vs Haploidentical (HR 2.32, 95% CI: 0.581–9.26, p= 0.234), possibly related with our small sample.
Conclusion
Our results in more than 1000 transplant demonstrated that AHSCT2 is rarely indicated and confirm the poor prognosis reported by multicenter and single center experiences. Despite new management strategies for allogeneic transplants, mortality and relapse rates after AHSCT2 remain high. However, is a good treatment option for patients with late relapses and for those who achieve CR before second transplant. For earlier relapses and no chemosensitive patients, other options are required. Efforts should be made in identifying new strategies for these patients.
Keyword(s): Allogeneic hematopoietic stem cell transplant, Graft-versus-host disease (GVHD), Leukemia, Relapse
Abstract: EP1253
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Allogeneic hematopoietic stem cell transplantation (AHSCT) is a curative option in hematological malignancies. However, relapse is the first cause of transplant failure. Risk of relapse depends on disease and transplant characteristics 1-4.
The best approach after relapse hasn´t been defined and as prognosis is so poor, AHSCT2 is considered for some patients mainly if relapse after 6 months and are fit enough. Many questions remain regarding the best strategy for AHSCT2.
Aims
The aim of this study was to analyze our center´s experience in patients receiving AHSCT2 in order to identify possible factors to improve management and OS in these patients.
Methods
From 1995, 1119 patients have received an AHSCT in our Unit. Of them, 53 (4.7%) received AHSCT2. A retrospective analysis of data included in our Transplant data base was performed. Statistical analysis was performed with SPSS.
Results
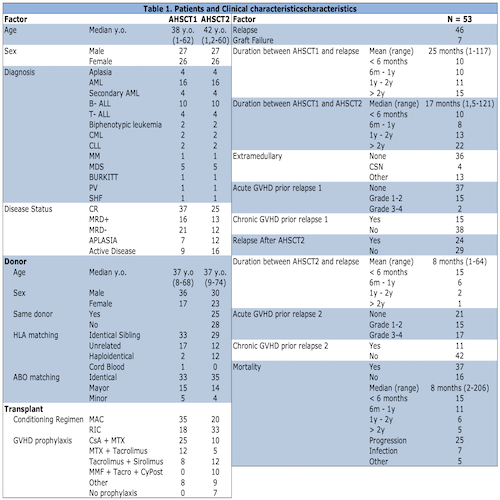
Patients’ characteristics are summarized in Table 1. Median age at AHSCT2 was 35 years old (range 1 to 65). Mean time between AHSCT1 and relapse was 25 months (range 1 to 117) and median time between AHSCTs was 17 months (range 1.5 to 121) Cause of AHSCT2 was relapse for 46/53 (87%) patients and graft failure for 7/53 (13%), of this latter 6/7 (86%) are still alive with graft recovery.
Most frequent diagnosis was primary acute leukemia (57%) (AML= 30%, B- ALL= 20% and T- ALL= 7%). Disease status at AHSCT2 was CR 25/53 (47%) (12/25 (48%) MRD negative), aplasia 12/53 (23%) and active disease (AD) in 16/53 (30%) respectively. Conditioning regimen was Myeloablative (MAC) in 35/53 (66%) for AHSCT 1 and in 20/53 (38%) of the patients for AHSCT2.
Donor was the same in 25/53 (47%) of the transplants. Donor was HLA identical sibling in 29/53 (55%), unrelated in 12/53 (23%) and haploidentical in 12/53 (23%) respectively.
With a median follow-up of 11 months (range 2 to 253) and 54 months (range 3 to 253) for surviving patients, 37 patients have died and 16 (30%) are still alive, 15/16 (94%) disease free. 12/37 patients die due to causes different from progression with Non relapse mortality of 32%.
The 2- and 4-years OS was 39% (SD ± 0.070) and 34% (SD ± 0.069) and the 2- and 4- years PFS was 35% (SD ± 0.067) and 33% (SD ± 0.066) respectively.
Thirty- two (60%) patients presented acute GVHD (aGVHD), 97% involving skin and/or gut. 11/53 (21%) presented Chronic GVDH after AHSCT2.
In the multivariate analysis, the variables which influenced OS were CR vs AD at AHSCT2 (HR 7.96, 95% CI: 2.67–23.78, p <0.001), MAC vs RIC (HR 7.79, 95% CI: 2.55–23.85, p <0.001) and relapse <25 months vs >25 months after AHSCT1 (HR 18.16, 95% CI: 2.03–162.178, p=0.009). HLA matching had no statistically significant impact on OS Identical sibling vs Haploidentical (HR 2.32, 95% CI: 0.581–9.26, p= 0.234), possibly related with our small sample.
Conclusion
Our results in more than 1000 transplant demonstrated that AHSCT2 is rarely indicated and confirm the poor prognosis reported by multicenter and single center experiences. Despite new management strategies for allogeneic transplants, mortality and relapse rates after AHSCT2 remain high. However, is a good treatment option for patients with late relapses and for those who achieve CR before second transplant. For earlier relapses and no chemosensitive patients, other options are required. Efforts should be made in identifying new strategies for these patients.
Keyword(s): Allogeneic hematopoietic stem cell transplant, Graft-versus-host disease (GVHD), Leukemia, Relapse


