
Contributions
Abstract: EP1252
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Skin and soft tissue infections (SSTIs) refer to infections occurring in the skin, subcutaneous tissue, fascia and muscle. As immunocompromised hosts, transplantation patients are more likely to develop SSTIs. According to the Infectious Diseases Society of America (IDSA), SSTIs in immunocompromised patients should all be classified as severe. Several previous studies have analysed the epidemiology and risk factors of SSTIs in solid organ transplantation (OST) recipients. However, to date, no study has focused on SSTIs in haematopoietic stem cell transplantation (HSCT) recipients. The common pathogens, occurrence periods and anatomic sites and clinical outcomes of SSTIs in HSCT population remain unclear.
Aims
This retrospective study investigated the frequency, occurrence time, common anatomic locations, comorbidities and clinical outcomes of allo-HSCT recipients with SSTIs. Moreover, a prognostic model for allo-HSCT recipients with SSTIs was developed.
Methods
Allo-HSCT recipients developing SSTIs from pretreatment to 180 days after transplantation were included in our study. Pathogens including bacterium, fungus and virus were all involved. The patients’ baseline characteristics, infection profiles, synchronous comorbidities and clinical outcomes were recorded in. Comorbidity referred to diseases occurring within 7 days before and after the SSTI course. Acute kidney injury was defined as serum creatinine increased 1.5–1.9 times baseline or ≥0.3 mg/dl, or urine output <0.5 ml/kg/h for over 6 hours. Patients involved were divided into two groups according to their outcome: survivors and nonsurvivors at 12 months after HSCT. We compared the differences between the two groups and developed a prognostic model.
Results
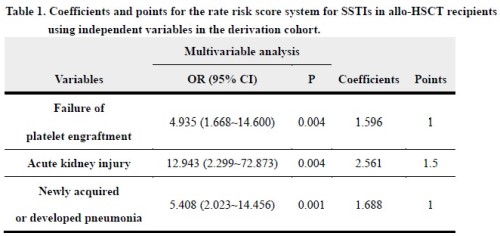
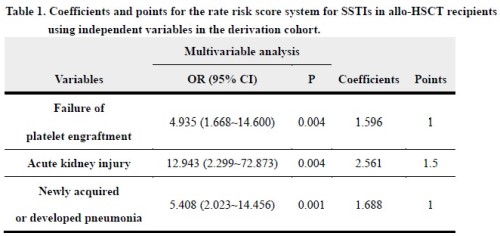
Two hundred twelve allo-HSCT recipients with 231 SSTIs were included from January 2005 to December 2019 at the Peking University Institute of Haematology, with a 12-month mortality of 27.4% (58/221). The median onset time of SSTI after transplantation was 10 days (from -9 to 179). Anal infection was the most common (19.4%, 45/231), while maxillofacial infection ranked second (18.6%, 43/231) and infection due to vascular devices ranked third (16.5%, 38/231). Pneumonia was the most common comorbidity of SSTI (23.8%, 55/231). Recipients who had undergone allo-HSCT after January 2014 were grouped as the derivation cohort, while others were grouped as the validation cohort. Failure of platelet engraftment, newly acquired or developed pneumonia and combined acute kidney injury were independent risk factors for 12-month death. According to the modelling coefficient magnitude of each factor, a risk score system was established (Table 1). The risk score was 1×failure of platelet engraftment+1.5×acute kidney injury+1×pneumonia. The patients’ 12-month mortality rose with the score increasing. The 12-month mortality rates at 0 points, 1 point and 1.5 points were 12.1%, 44.7% and 77.8%, respectively. The bootstrap internal and external validation showed good discrimination power with AUCs of 0.817 (95CI: 0.692-0.866) and 0.749 (95CI: 0.625-0.855) in the derivation and validation cohorts, respectively. Additionally, the calibration plot demonstrated high agreement between the estimated and observed risks of 12-month death in the study population. Furthermore, decision curve analysis indicated considerable clinical benefit for patients.
Conclusion
SSTIs are common complications in allo-HSCT recipients. Failure of platelet engraftment, combined pneumonia and acute kidney injury can predict the prognosis of patients.
Keyword(s): Allogeneic hematopoietic stem cell transplant, Infection, Outcome, Prognostic factor
Abstract: EP1252
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Skin and soft tissue infections (SSTIs) refer to infections occurring in the skin, subcutaneous tissue, fascia and muscle. As immunocompromised hosts, transplantation patients are more likely to develop SSTIs. According to the Infectious Diseases Society of America (IDSA), SSTIs in immunocompromised patients should all be classified as severe. Several previous studies have analysed the epidemiology and risk factors of SSTIs in solid organ transplantation (OST) recipients. However, to date, no study has focused on SSTIs in haematopoietic stem cell transplantation (HSCT) recipients. The common pathogens, occurrence periods and anatomic sites and clinical outcomes of SSTIs in HSCT population remain unclear.
Aims
This retrospective study investigated the frequency, occurrence time, common anatomic locations, comorbidities and clinical outcomes of allo-HSCT recipients with SSTIs. Moreover, a prognostic model for allo-HSCT recipients with SSTIs was developed.
Methods
Allo-HSCT recipients developing SSTIs from pretreatment to 180 days after transplantation were included in our study. Pathogens including bacterium, fungus and virus were all involved. The patients’ baseline characteristics, infection profiles, synchronous comorbidities and clinical outcomes were recorded in. Comorbidity referred to diseases occurring within 7 days before and after the SSTI course. Acute kidney injury was defined as serum creatinine increased 1.5–1.9 times baseline or ≥0.3 mg/dl, or urine output <0.5 ml/kg/h for over 6 hours. Patients involved were divided into two groups according to their outcome: survivors and nonsurvivors at 12 months after HSCT. We compared the differences between the two groups and developed a prognostic model.
Results
Two hundred twelve allo-HSCT recipients with 231 SSTIs were included from January 2005 to December 2019 at the Peking University Institute of Haematology, with a 12-month mortality of 27.4% (58/221). The median onset time of SSTI after transplantation was 10 days (from -9 to 179). Anal infection was the most common (19.4%, 45/231), while maxillofacial infection ranked second (18.6%, 43/231) and infection due to vascular devices ranked third (16.5%, 38/231). Pneumonia was the most common comorbidity of SSTI (23.8%, 55/231). Recipients who had undergone allo-HSCT after January 2014 were grouped as the derivation cohort, while others were grouped as the validation cohort. Failure of platelet engraftment, newly acquired or developed pneumonia and combined acute kidney injury were independent risk factors for 12-month death. According to the modelling coefficient magnitude of each factor, a risk score system was established (Table 1). The risk score was 1×failure of platelet engraftment+1.5×acute kidney injury+1×pneumonia. The patients’ 12-month mortality rose with the score increasing. The 12-month mortality rates at 0 points, 1 point and 1.5 points were 12.1%, 44.7% and 77.8%, respectively. The bootstrap internal and external validation showed good discrimination power with AUCs of 0.817 (95CI: 0.692-0.866) and 0.749 (95CI: 0.625-0.855) in the derivation and validation cohorts, respectively. Additionally, the calibration plot demonstrated high agreement between the estimated and observed risks of 12-month death in the study population. Furthermore, decision curve analysis indicated considerable clinical benefit for patients.
Conclusion
SSTIs are common complications in allo-HSCT recipients. Failure of platelet engraftment, combined pneumonia and acute kidney injury can predict the prognosis of patients.
Keyword(s): Allogeneic hematopoietic stem cell transplant, Infection, Outcome, Prognostic factor


