
Contributions
Abstract: EP1242
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Allogeneic hematopoietic cell transplantation is a well-established treatment modality for multiple hematological diseases, however a significant risk of complications remains. It is performed only in specialized centers and patients necessitate intense follow-up care posttransplant which is usually performed at the transplant center, in turn leading to long travel times for patients. It is conceivable that travel burden could impair the quality of posttransplant care, as has been shown in other healthcare settings. Previous retrospective studies conducted in North America have shown contrasting results regarding the impact of travel distance on outcome. To reduce the burden of travel time to our center, whenever possible we offer shared care posttransplant meaning that patients can receive some or in selected cases all follow-up visits with other health care providers with which we have an established collaboration.
Aims
Due to the situation at our center with long travel times on the one hand and an established shared care model posttransplant on the other hand, we were interested in analyzing the impact of distance and posttransplant care model on outcome parameters.
Methods
We conducted a retrospective analysis of 678 patients who received a first allogeneic transplantation at the University Hospital of Basel between January 2008 and December 2017. Pediatric patients were excluded. All study participants gave written informed consent. Since the intention to provide shared care posttransplant was not collected prospectively, patients who did not receive shared care presumably also included those that died before they could continue to outpatient care or were considered too sick. For this reason, we performed selected analyses in a landmark population of patients alive at day 180.
Results
Median age at transplant was 53y (range 19-75), 416 (61%) were male. The most common disease was acute leukemia (n=329, 49%). The majority of patients had an unrelated donor (n=379, 56%) and a myeloablative conditioning regimen (n=467, 69%). The median follow-up of survivors was 1750 days while 57% of the patients were still alive after 3 years.
Median travel time by car and public transport to the transplant center was 67min and 112min respectively, and 56% and 78% of patients had a travel time of over 1h by car and public transport respectively.
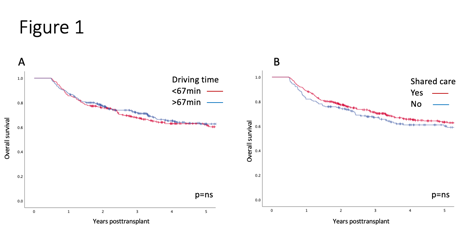
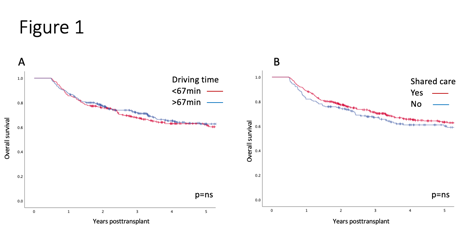
Of the patients in the landmark population alive at day 180 (n=553), 375 (68%) received shared care, and 277 (91%) of those with a driving time >1h. There was no difference in overall survival (OS) for patients with driving time over or under the median or for those receiving shared care posttransplant versus not (Figure 1). A multivariable analysis including patient and transplant characteristics confirmed the lack of association between driving time and receiving shared care with OS in the landmark population. Patients alive at one year receiving shared care had significantly less visits at the transplant center with a median of 12 versus 22 visits (p<0.001) between day 100 and day 365.
Conclusion
Our study demonstrates that within the framework of shared care, increasing distance to the transplant center does not negatively impact outcome and that the burden of prolonged travel time for patients can be significantly reduced. While acknowledging the limits of a retrospective analysis, to our knowledge, this is the first such study performed in Europe, and we believe it will help optimize post-transplant follow-up and is an important contribution to the growing field of health services research.
Keyword(s): Allogeneic, Follow-up, Health care
Abstract: EP1242
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Allogeneic hematopoietic cell transplantation is a well-established treatment modality for multiple hematological diseases, however a significant risk of complications remains. It is performed only in specialized centers and patients necessitate intense follow-up care posttransplant which is usually performed at the transplant center, in turn leading to long travel times for patients. It is conceivable that travel burden could impair the quality of posttransplant care, as has been shown in other healthcare settings. Previous retrospective studies conducted in North America have shown contrasting results regarding the impact of travel distance on outcome. To reduce the burden of travel time to our center, whenever possible we offer shared care posttransplant meaning that patients can receive some or in selected cases all follow-up visits with other health care providers with which we have an established collaboration.
Aims
Due to the situation at our center with long travel times on the one hand and an established shared care model posttransplant on the other hand, we were interested in analyzing the impact of distance and posttransplant care model on outcome parameters.
Methods
We conducted a retrospective analysis of 678 patients who received a first allogeneic transplantation at the University Hospital of Basel between January 2008 and December 2017. Pediatric patients were excluded. All study participants gave written informed consent. Since the intention to provide shared care posttransplant was not collected prospectively, patients who did not receive shared care presumably also included those that died before they could continue to outpatient care or were considered too sick. For this reason, we performed selected analyses in a landmark population of patients alive at day 180.
Results
Median age at transplant was 53y (range 19-75), 416 (61%) were male. The most common disease was acute leukemia (n=329, 49%). The majority of patients had an unrelated donor (n=379, 56%) and a myeloablative conditioning regimen (n=467, 69%). The median follow-up of survivors was 1750 days while 57% of the patients were still alive after 3 years.
Median travel time by car and public transport to the transplant center was 67min and 112min respectively, and 56% and 78% of patients had a travel time of over 1h by car and public transport respectively.
Of the patients in the landmark population alive at day 180 (n=553), 375 (68%) received shared care, and 277 (91%) of those with a driving time >1h. There was no difference in overall survival (OS) for patients with driving time over or under the median or for those receiving shared care posttransplant versus not (Figure 1). A multivariable analysis including patient and transplant characteristics confirmed the lack of association between driving time and receiving shared care with OS in the landmark population. Patients alive at one year receiving shared care had significantly less visits at the transplant center with a median of 12 versus 22 visits (p<0.001) between day 100 and day 365.
Conclusion
Our study demonstrates that within the framework of shared care, increasing distance to the transplant center does not negatively impact outcome and that the burden of prolonged travel time for patients can be significantly reduced. While acknowledging the limits of a retrospective analysis, to our knowledge, this is the first such study performed in Europe, and we believe it will help optimize post-transplant follow-up and is an important contribution to the growing field of health services research.
Keyword(s): Allogeneic, Follow-up, Health care


