
Contributions
Abstract: EP1241
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Allo-HSCT is accompanied by different complications including infections, graft-versus-host disease (GVHD) that require constant follow-up. Increased rate of HLA-mismatched allo-HSCT may be associated with higher hospital readmissions rate.
Aims
We studied the impact of immune status (T-, B- and natural killer lymphocytes, or NK-cells) in patients (pts) after allo-HSCT within the period from +6 to +12 months (mths) after transplantation for assessment of hospital readmission risk.
Methods
51 pts were included in the study (male=23, female=28). Median age 41 (min – 20, max – 70). Pts had diagnosis: AMLs (n=28), ALLs (n=10), NHLs (n=5), CLL (n=1), primary myelofibrosis (n=2), MDS (n=3), aplastic anemia (n=2). 8 pts (16%) had mismatched unrelated donors, 19 pts (37%) had mismatched related donors, 6 pts (12%) had haploidentical, 18 pts (35%) had matched related donors. 24 pts were transplanted with PBSC, 27 - with bone marrow. Myeloablative or reduced-intensity conditioning regimens were performed in 14 (27%) and 37 (73%) pts, respectively. Flow cytometry analysis was performed on BD FACS Canto II device (Becton Dickinson, USA) with BD Multitest™ 6-color TBNK kit to define Т-cells, Т-helpers, cytotoxic T-lymphocytes, NK-cells and В-cells on +6, +9, +12 mths. The two-platform method was used to determine an absolute lymphocytic subpopulation count. Mann–Whitney U test used for nonparametric data analysis. A p-value was less than cutoff 0.05 was considered significant. ROC-analysis was performed to determine parameters, which affect readmission rate. Multivariate analysis (MVA) was used to determine the relating probability of readmission with gender, age of pts, type of donors, type of grafts, GVHDs, numbers of T-helpers, B-cells, NKs.
Results
From +6 to +9 mths 11 pts (29.7%) were hospitalized due to GVHD, 4 pts (10.8%) were hospitalized due to infections and 22 pts (59.5%) due to other reasons. From +9 to +12 mths hospital readmissions causes were: chronic GVHD (n=13, 41.9%), infections (n=2, 6.5%), relapses (n=4, 12.9%) and other reasons (n=12, 38.7%).
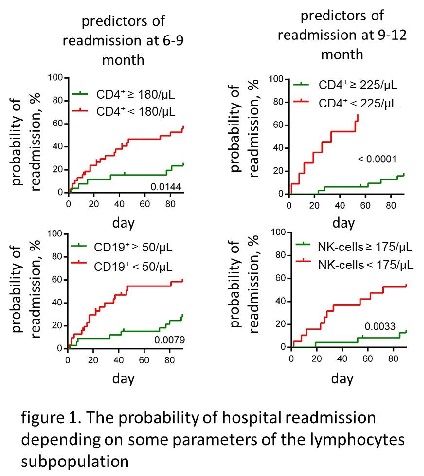
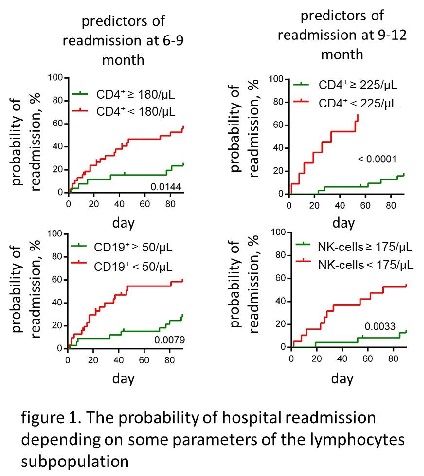
According to thresholds determined by ROC analysis pts were divided into two groups. The probability of readmissions in the period from +6 to +9 mths were: 55% for pts with the absolute number of T-helpers less than 180/μL and 23% for pts with the absolute number of T-helpers more than 180/μL (p=0.0144); 58% for pts with B-cells less than 50/μL and 27% for pts with B-cells more than 50/μL (p=0.0079). The probability of readmissions in the period from +9 to +12 mths were: 72% for pts with the absolute number of T-helpers less than 225/μL and 16% for pts with the absolute number of T-helpers more than 225/μL (p<0.0001); 52% for pts with NKs less than 175/μL and 18% for pts with NKs less than 175/μL (p=0.0033) (figure 1).
In MVA probability of readmissions weren’t related to gender, age of pts, donor’s type, graft type, GVHD. But probability of readmissions at +9 mths was significantly associated with the absolute number of T-helpers (for pts with the absolute number of CD4<180/μL at +6 mths (p=0.0435) and for pts with the absolute number of CD4<180/μL at +9 mths (p=0.0157)) and B-cells (p = 0.0184 for pts with the absolute number of CD19<50/μL at +9 mths).
Conclusion
The absolute number of NK cells, B-cells and Т-helpers can reflect the quality of immune reconstitution after allo-HSCT. The low level of these cells may predict high readmission risk in the post-engraftment period after allo-HSCT at different time points disregarding gender, age of pts, donor’s type, graft type, GVHD.
Keyword(s): Allogeneic hematopoietic stem cell transplant, Flow cytometry, Immune reconstitution
Abstract: EP1241
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Allo-HSCT is accompanied by different complications including infections, graft-versus-host disease (GVHD) that require constant follow-up. Increased rate of HLA-mismatched allo-HSCT may be associated with higher hospital readmissions rate.
Aims
We studied the impact of immune status (T-, B- and natural killer lymphocytes, or NK-cells) in patients (pts) after allo-HSCT within the period from +6 to +12 months (mths) after transplantation for assessment of hospital readmission risk.
Methods
51 pts were included in the study (male=23, female=28). Median age 41 (min – 20, max – 70). Pts had diagnosis: AMLs (n=28), ALLs (n=10), NHLs (n=5), CLL (n=1), primary myelofibrosis (n=2), MDS (n=3), aplastic anemia (n=2). 8 pts (16%) had mismatched unrelated donors, 19 pts (37%) had mismatched related donors, 6 pts (12%) had haploidentical, 18 pts (35%) had matched related donors. 24 pts were transplanted with PBSC, 27 - with bone marrow. Myeloablative or reduced-intensity conditioning regimens were performed in 14 (27%) and 37 (73%) pts, respectively. Flow cytometry analysis was performed on BD FACS Canto II device (Becton Dickinson, USA) with BD Multitest™ 6-color TBNK kit to define Т-cells, Т-helpers, cytotoxic T-lymphocytes, NK-cells and В-cells on +6, +9, +12 mths. The two-platform method was used to determine an absolute lymphocytic subpopulation count. Mann–Whitney U test used for nonparametric data analysis. A p-value was less than cutoff 0.05 was considered significant. ROC-analysis was performed to determine parameters, which affect readmission rate. Multivariate analysis (MVA) was used to determine the relating probability of readmission with gender, age of pts, type of donors, type of grafts, GVHDs, numbers of T-helpers, B-cells, NKs.
Results
From +6 to +9 mths 11 pts (29.7%) were hospitalized due to GVHD, 4 pts (10.8%) were hospitalized due to infections and 22 pts (59.5%) due to other reasons. From +9 to +12 mths hospital readmissions causes were: chronic GVHD (n=13, 41.9%), infections (n=2, 6.5%), relapses (n=4, 12.9%) and other reasons (n=12, 38.7%).
According to thresholds determined by ROC analysis pts were divided into two groups. The probability of readmissions in the period from +6 to +9 mths were: 55% for pts with the absolute number of T-helpers less than 180/μL and 23% for pts with the absolute number of T-helpers more than 180/μL (p=0.0144); 58% for pts with B-cells less than 50/μL and 27% for pts with B-cells more than 50/μL (p=0.0079). The probability of readmissions in the period from +9 to +12 mths were: 72% for pts with the absolute number of T-helpers less than 225/μL and 16% for pts with the absolute number of T-helpers more than 225/μL (p<0.0001); 52% for pts with NKs less than 175/μL and 18% for pts with NKs less than 175/μL (p=0.0033) (figure 1).
In MVA probability of readmissions weren’t related to gender, age of pts, donor’s type, graft type, GVHD. But probability of readmissions at +9 mths was significantly associated with the absolute number of T-helpers (for pts with the absolute number of CD4<180/μL at +6 mths (p=0.0435) and for pts with the absolute number of CD4<180/μL at +9 mths (p=0.0157)) and B-cells (p = 0.0184 for pts with the absolute number of CD19<50/μL at +9 mths).
Conclusion
The absolute number of NK cells, B-cells and Т-helpers can reflect the quality of immune reconstitution after allo-HSCT. The low level of these cells may predict high readmission risk in the post-engraftment period after allo-HSCT at different time points disregarding gender, age of pts, donor’s type, graft type, GVHD.
Keyword(s): Allogeneic hematopoietic stem cell transplant, Flow cytometry, Immune reconstitution


