
Contributions
Abstract: EP1240
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Reactivation of cytomegalovirus (CMV) or Epstein-Barr virus (EBV) is common after hematopoietic stem cell transplantation (HSCT). Previous researches have demonstrated that either CMV or EBV reactivation is associated with poor outcomes of HSCT. However, few studies investigate the impact of CMV and EBV co-reactivation after HSCT.
Aims
Our aim was to described clinical characteristics of patients with co-reactivation of CMV and EBV (defined as CMV and EBV viremia occur at the same period of time), research the impact of such co-reactivation on prognosis and identify associated risk factors.
Methods
We conducted a longitudinal study of 247 patients who underwent first HSCT in our center between July 2015 and June 2016. Of these 247 patients, different conditioning regimen were performed according to their different underlying disease. They received uniform CMV and EBV monitoring and therapy, as well as graft-versus-host disease (GVHD) prophylaxis. Peripheral blood samples were collected from the recipients at 30, 60 and 90 days after HSCT for immunophenotyping. Co-reactivation of CMV and EBV was defined as the detection of EBV or CMV viremia during CMV or EBV viremia, respectively. The time of co-reactivation was defined as the day when viremia of the first virus was identified. Univariate and multivariate analysis and survival analysis were performed to elucidate the impact of such co-reactivation on prognosis and identify associated risk factors.
Results
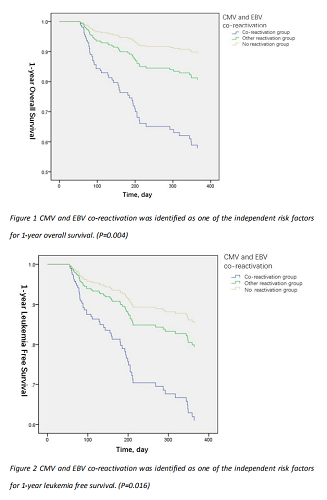
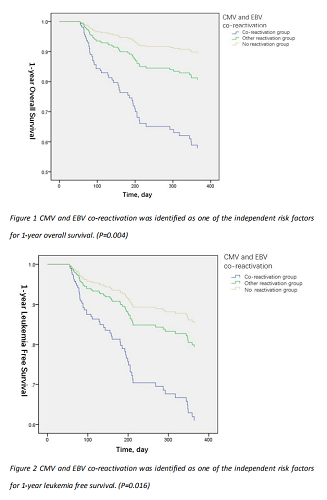
A total of 24 (9.7%) patients had CMV and EBV co-reactivation of these 247 patients. These patients showed higher incidence of viral pneumonitis (P=0.005). Patients with CMV and EBV co-reactivation had significant lower 1-year overall survival (OS) (P=0.004) and lower 1-year leukemia free survival (LFS) (P=0.016). Our further analysis suggested that duration of CMV (P=0.014), EBV (P<0.001), and CD4+CD25+ T cell counts at day 30 post-transplantation (P=0.05) are independent risk factors of virus co-reactivation.
Conclusion
Patients who developed co-reactivation of CMV and EBV had poor prognosis in terms of lower 1-year OS and LFS, and the CMV and EBV co-reactivation was associated with prolonged CMV or EBV duration and poor CD4+CD25+ T cell reconstitution at day 30 post-transplantation, which may provide an alternative way to prevent CMV and EBV reactivation in HSCT patients.
Keyword(s): CMV, EBV, Immune reconstitution, Stem cell transplant
Abstract: EP1240
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Reactivation of cytomegalovirus (CMV) or Epstein-Barr virus (EBV) is common after hematopoietic stem cell transplantation (HSCT). Previous researches have demonstrated that either CMV or EBV reactivation is associated with poor outcomes of HSCT. However, few studies investigate the impact of CMV and EBV co-reactivation after HSCT.
Aims
Our aim was to described clinical characteristics of patients with co-reactivation of CMV and EBV (defined as CMV and EBV viremia occur at the same period of time), research the impact of such co-reactivation on prognosis and identify associated risk factors.
Methods
We conducted a longitudinal study of 247 patients who underwent first HSCT in our center between July 2015 and June 2016. Of these 247 patients, different conditioning regimen were performed according to their different underlying disease. They received uniform CMV and EBV monitoring and therapy, as well as graft-versus-host disease (GVHD) prophylaxis. Peripheral blood samples were collected from the recipients at 30, 60 and 90 days after HSCT for immunophenotyping. Co-reactivation of CMV and EBV was defined as the detection of EBV or CMV viremia during CMV or EBV viremia, respectively. The time of co-reactivation was defined as the day when viremia of the first virus was identified. Univariate and multivariate analysis and survival analysis were performed to elucidate the impact of such co-reactivation on prognosis and identify associated risk factors.
Results
A total of 24 (9.7%) patients had CMV and EBV co-reactivation of these 247 patients. These patients showed higher incidence of viral pneumonitis (P=0.005). Patients with CMV and EBV co-reactivation had significant lower 1-year overall survival (OS) (P=0.004) and lower 1-year leukemia free survival (LFS) (P=0.016). Our further analysis suggested that duration of CMV (P=0.014), EBV (P<0.001), and CD4+CD25+ T cell counts at day 30 post-transplantation (P=0.05) are independent risk factors of virus co-reactivation.
Conclusion
Patients who developed co-reactivation of CMV and EBV had poor prognosis in terms of lower 1-year OS and LFS, and the CMV and EBV co-reactivation was associated with prolonged CMV or EBV duration and poor CD4+CD25+ T cell reconstitution at day 30 post-transplantation, which may provide an alternative way to prevent CMV and EBV reactivation in HSCT patients.
Keyword(s): CMV, EBV, Immune reconstitution, Stem cell transplant


