
Contributions
Abstract: EP1236
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Veno-occlusive disease (VOD), or sinusoidal obstruction syndrome, is a rare liver disorder which is associated with high morbidity and mortality. Patients with hematological malignancies are at particularly high risk of developing VOD following antineoplastic treatment, especially among those who had hemopoietic stem cell transplantation (HSCT).
Aims
To apply an adapted algorithm based on the Seattle/Baltimore diagnostic criteria to identify VOD patients among adult hematological cancer patients and a subcohort of patients with leukemia in England, and to describe their demographic, clinical characteristics, and mortality.
Methods
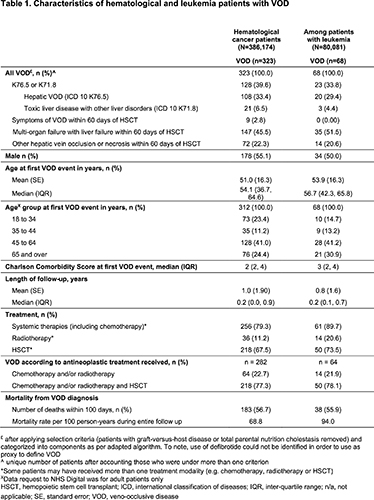
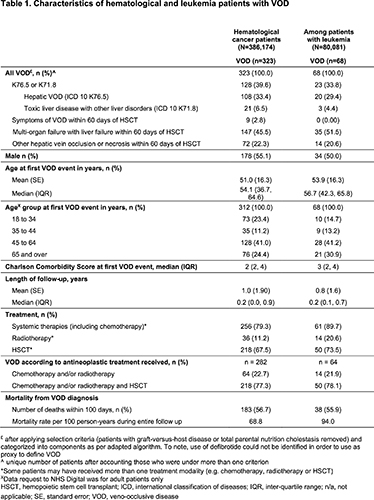
This retrospective observational study utilized the Hospital Episode Statistics (HES) inpatients, outpatients, and critical care ‘pseudonymized’ datasets (NHS Digital, England) as its source of adult hematological cancer patients, including a subcohort with leukemia, identified between 1/1/2010 and 31/3/2020. An algorithm to identify VOD was applied based on the Baltimore/Seattle diagnostic criteria and other clinical features of the disease (with a breakdown of its components shown in Table 1); adults with chronic graft-versus-host disease (GVHD) or total parenteral nutrition (TPN) cholestasis were not included. Patients with VOD were followed up from diagnosis of VOD (index date) until the earliest occurrence of death or end of study period.
Results
A total of 386,174 adults with hematological cancers (mean age: 67.9; males: 57.9%), including a subcohort of 80,081 patients with leukemia (mean age: 70.7; males: 60.4%), were identified within the HES datasets during study period. Overall, the adapted algorithm identified 323 (8 per 10,000; mean age: 51.0; males: 55.1%) patients with VOD in the hematological cancer cohort, and 68 (8 per 10,000; mean age: 53.9; males: 50.0%) in the leukemia subcohort (Table 1). The majority (~41%) developed VOD between 45 and 64 years of age. Overall, prior systemic antineoplastic therapies (inc. chemotherapy), radiotherapy and HSCT were received by 79.3%, 11.2% and 67.5% of hematological cancer patients and 89.7%, 20.6% and 73.5% of leukemia patients, respectively. Antineoplastic treatments were received by 282 hematological cancer patients who developed VOD and among them 218 (77.3%) had prior HSCT. Within the leukemia subcohort, 50 of 64 (78.1%) VOD patients had prior HSCT. Among patients with VOD, 56.7% (hematological cancer patients) and 55.9% (leukemia patients) died within 100 days of developing the disease. The mortality rates following VOD were 68.8 and 94.0 per 100 person-years, among hematological cancer patients and leukemia subcohort, respectively.
Conclusion
This study identified a similar proportion of VOD patients (8 per 10,000) in the overall hematological cancer cohort as in the leukemia subcohort. It should be noted that the incidence of VOD is representative of the calculations that were based on this study’s adapted algorithm. Among patients who were treated for their hematological cancers and subsequently developed VOD, this particular algorithm identified that three quarters had prior HSCT in their treatment strategies. The high mortality rate among patients with VOD in England suggests a clear need to focus research and clinical efforts to identify the disease promptly, develop risk-profiling methodology and improve patients’ survival.
Keyword(s): Hematological malignancy, Hematopoietic stem cell, Leukemia, Veno-occlusive disease
Abstract: EP1236
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Veno-occlusive disease (VOD), or sinusoidal obstruction syndrome, is a rare liver disorder which is associated with high morbidity and mortality. Patients with hematological malignancies are at particularly high risk of developing VOD following antineoplastic treatment, especially among those who had hemopoietic stem cell transplantation (HSCT).
Aims
To apply an adapted algorithm based on the Seattle/Baltimore diagnostic criteria to identify VOD patients among adult hematological cancer patients and a subcohort of patients with leukemia in England, and to describe their demographic, clinical characteristics, and mortality.
Methods
This retrospective observational study utilized the Hospital Episode Statistics (HES) inpatients, outpatients, and critical care ‘pseudonymized’ datasets (NHS Digital, England) as its source of adult hematological cancer patients, including a subcohort with leukemia, identified between 1/1/2010 and 31/3/2020. An algorithm to identify VOD was applied based on the Baltimore/Seattle diagnostic criteria and other clinical features of the disease (with a breakdown of its components shown in Table 1); adults with chronic graft-versus-host disease (GVHD) or total parenteral nutrition (TPN) cholestasis were not included. Patients with VOD were followed up from diagnosis of VOD (index date) until the earliest occurrence of death or end of study period.
Results
A total of 386,174 adults with hematological cancers (mean age: 67.9; males: 57.9%), including a subcohort of 80,081 patients with leukemia (mean age: 70.7; males: 60.4%), were identified within the HES datasets during study period. Overall, the adapted algorithm identified 323 (8 per 10,000; mean age: 51.0; males: 55.1%) patients with VOD in the hematological cancer cohort, and 68 (8 per 10,000; mean age: 53.9; males: 50.0%) in the leukemia subcohort (Table 1). The majority (~41%) developed VOD between 45 and 64 years of age. Overall, prior systemic antineoplastic therapies (inc. chemotherapy), radiotherapy and HSCT were received by 79.3%, 11.2% and 67.5% of hematological cancer patients and 89.7%, 20.6% and 73.5% of leukemia patients, respectively. Antineoplastic treatments were received by 282 hematological cancer patients who developed VOD and among them 218 (77.3%) had prior HSCT. Within the leukemia subcohort, 50 of 64 (78.1%) VOD patients had prior HSCT. Among patients with VOD, 56.7% (hematological cancer patients) and 55.9% (leukemia patients) died within 100 days of developing the disease. The mortality rates following VOD were 68.8 and 94.0 per 100 person-years, among hematological cancer patients and leukemia subcohort, respectively.
Conclusion
This study identified a similar proportion of VOD patients (8 per 10,000) in the overall hematological cancer cohort as in the leukemia subcohort. It should be noted that the incidence of VOD is representative of the calculations that were based on this study’s adapted algorithm. Among patients who were treated for their hematological cancers and subsequently developed VOD, this particular algorithm identified that three quarters had prior HSCT in their treatment strategies. The high mortality rate among patients with VOD in England suggests a clear need to focus research and clinical efforts to identify the disease promptly, develop risk-profiling methodology and improve patients’ survival.
Keyword(s): Hematological malignancy, Hematopoietic stem cell, Leukemia, Veno-occlusive disease


