Contributions
Abstract: EP1234
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Haploidentical HLA stem cell transplantation (haplo-HSCT) is increasingly being used as part of the treatment of hematological malignancies lacking a suitable HLA-matched donor. Cytokine release syndrome (CRS) is a systemic inflammatory response with aberrant immune activation and hyperstimulation which has been described in a number of clinical settings, including haplo-HSCT. However, clinical impact of CRS on these patients is controversial.
During COVID-19 pandemic, graft cryopreservation in haplo-HSCT has increased in our centre. As a result, we clinically noticed a change in CRS onset in these patients.
Aims
To identify novel CRS features that might have a prognostic impact on haplo-HSCT, as well as to determine if graft cryopreservation might influence any of those features.
Methods
A cohort of 154 patients undergoing allogeneic stem cell transplantation in 2019 and 2020 in our centre, from which 51 patients receiving peripheral blood haplo-HSCT from 1st February 2019 to 31st December 2020 were selected. Two of them were excluded for the CRS analysis due to relevant microbiological isolation close to the infusion date and impossibility to distinguish between infectious and CRS fever. CRS was graded according to the ASBMT consensus.
Results
The median age was 51 years (range 17-72), 59% were male. Median follow-up was 359 days for alive patients. Hematopoietic Cell Transplantation Comorbidity Index (HCT-CI) was low risk in 45%, intermediate risk in 22% and high risk in 33%. Most patients (71%) had an intermediate Disease Risk Index (DRI). Conditioning regimen was myeloablative in 12 (24%). 84% of the patients presented with CRS after haplo-HSCT (71% of them occurred in the first 48 hours after infusion). CRS was mild in most patients (grade 1 in 29 (71%) and grade 2 in 12 (29%); no grade 3 CRS or further occurred. Graft cryopreservation accounted for 13 (25%) patients.
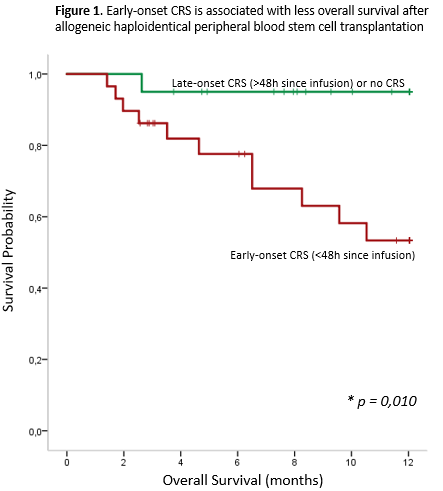
Early-onset CRS (<48h since stem cell infusion) was associated with lower overall survival (Figure 1, p=0,01), as well as lower event free survival (relapse or death, p=0,03) when compared with the remaining patients in a univariate analysis. Non-myeloablative conditioning was associated with a higher proportion of early-onset CRS (74% vs 9%, p<0,001) as well as age >60 years (80% vs 45% p=0,014). It should be noted that age >60 years did not impact on overall survival in the first year following haplo-HSCT in our patients (p=0,485). We also found an interesting trend between graft cryopreservation and early-onset CRS (only 38% of patients with graft cryopreservation presented early-onset CRS, whereas 67% of patients with fresh graft did so, p=0,075).
Cryopreservation was related to less proportion of CRS grade ≥2 (0% vs 33%, p=0,014) and it did not impact on engraftment, overall survival nor graft versus receptor disease rate or severity in our patients. Patients with refractory disease prior to transplantation presented higher rates of CRS grade ≥2 (75% vs 20%, p=0,041). Moreover, a trend was observed for mononucleated cell count >8 x 108 (37% vs 14%, p=0,067). However, CRS grade ≥2 did not impact on overall survival in our patients (p=0,251).
Conclusion
Early-onset CRS is associated with less overall survival and less event-free survival following the first year after haplo-HSCT. Cryopreservation is associated with less CRS grade ≥2 probability and might also reduce the chance of developing early-onset CRS.
Keyword(s): Cryopreservation, Haploidentical stem cell transplantation, Survival
Abstract: EP1234
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Haploidentical HLA stem cell transplantation (haplo-HSCT) is increasingly being used as part of the treatment of hematological malignancies lacking a suitable HLA-matched donor. Cytokine release syndrome (CRS) is a systemic inflammatory response with aberrant immune activation and hyperstimulation which has been described in a number of clinical settings, including haplo-HSCT. However, clinical impact of CRS on these patients is controversial.
During COVID-19 pandemic, graft cryopreservation in haplo-HSCT has increased in our centre. As a result, we clinically noticed a change in CRS onset in these patients.
Aims
To identify novel CRS features that might have a prognostic impact on haplo-HSCT, as well as to determine if graft cryopreservation might influence any of those features.
Methods
A cohort of 154 patients undergoing allogeneic stem cell transplantation in 2019 and 2020 in our centre, from which 51 patients receiving peripheral blood haplo-HSCT from 1st February 2019 to 31st December 2020 were selected. Two of them were excluded for the CRS analysis due to relevant microbiological isolation close to the infusion date and impossibility to distinguish between infectious and CRS fever. CRS was graded according to the ASBMT consensus.
Results
The median age was 51 years (range 17-72), 59% were male. Median follow-up was 359 days for alive patients. Hematopoietic Cell Transplantation Comorbidity Index (HCT-CI) was low risk in 45%, intermediate risk in 22% and high risk in 33%. Most patients (71%) had an intermediate Disease Risk Index (DRI). Conditioning regimen was myeloablative in 12 (24%). 84% of the patients presented with CRS after haplo-HSCT (71% of them occurred in the first 48 hours after infusion). CRS was mild in most patients (grade 1 in 29 (71%) and grade 2 in 12 (29%); no grade 3 CRS or further occurred. Graft cryopreservation accounted for 13 (25%) patients.
Early-onset CRS (<48h since stem cell infusion) was associated with lower overall survival (Figure 1, p=0,01), as well as lower event free survival (relapse or death, p=0,03) when compared with the remaining patients in a univariate analysis. Non-myeloablative conditioning was associated with a higher proportion of early-onset CRS (74% vs 9%, p<0,001) as well as age >60 years (80% vs 45% p=0,014). It should be noted that age >60 years did not impact on overall survival in the first year following haplo-HSCT in our patients (p=0,485). We also found an interesting trend between graft cryopreservation and early-onset CRS (only 38% of patients with graft cryopreservation presented early-onset CRS, whereas 67% of patients with fresh graft did so, p=0,075).
Cryopreservation was related to less proportion of CRS grade ≥2 (0% vs 33%, p=0,014) and it did not impact on engraftment, overall survival nor graft versus receptor disease rate or severity in our patients. Patients with refractory disease prior to transplantation presented higher rates of CRS grade ≥2 (75% vs 20%, p=0,041). Moreover, a trend was observed for mononucleated cell count >8 x 108 (37% vs 14%, p=0,067). However, CRS grade ≥2 did not impact on overall survival in our patients (p=0,251).
Conclusion
Early-onset CRS is associated with less overall survival and less event-free survival following the first year after haplo-HSCT. Cryopreservation is associated with less CRS grade ≥2 probability and might also reduce the chance of developing early-onset CRS.
Keyword(s): Cryopreservation, Haploidentical stem cell transplantation, Survival