
Contributions
Abstract: EP1231
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
MCL has been associated with poor prognosis, chemorefractoriness and older median age at diagnosis. For transplant-eligible patients, clinical outcome improves using intensive cytarabine-based induction, followed by autologous stem cell transplant (ASCT). Recently, new approaches with anti-CD20 maintenance, new target drugs or new ways of immunotherapy such as CARTs are changing the therapeutic landscape. Allo-SCT is a curative option for selected patients but with significant non-relapse mortality (NRM).
Aims
Our objective was to analyze long-term results in patients receiving allo-SCT in Spain.
Methods
We performed a retrospective multicenter study including patients from centers of GETH/GELTAMO with relapsed/refractory (R/R) MCL treated with allo-SCT from March 1995 to February 2020. The primary endpoints were event-free survival (EFS), overall survival (OS), NRM and cumulative incidence (CI) of relapse and graft versus host disease (GVHD).
Results
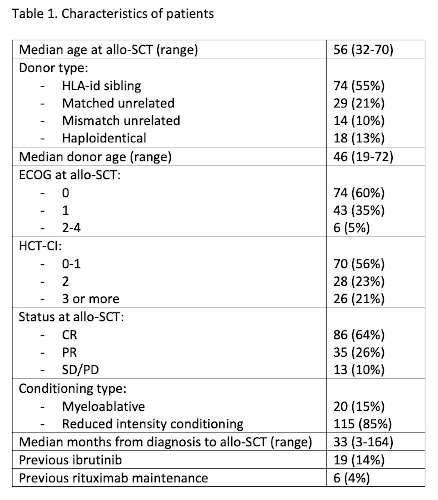
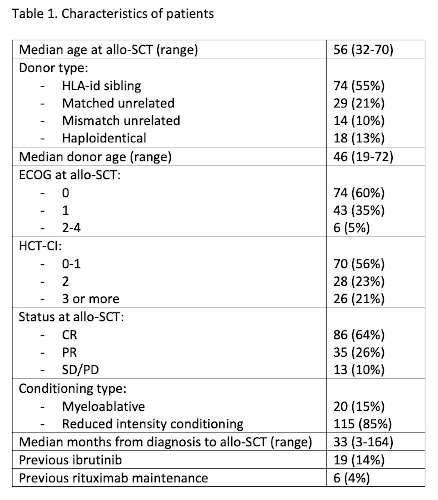
We included one-hundred and thirty-five patients with R/R MCL that fulfilled the inclusion criteria (Table 1). Median age was 56 years (27% >60 years); 49% had previous ASCT and median number of previous lines of therapy were 2 (1-8). Disease status at allo-SCT was complete response (CR) in 64%, partial response (PR) in 26% and stable/progressive disease (SD/PD) in 10%. Most patients (85%) received reduced intensity conditioning (RIC). After a median follow-up of 68 months (2-247), 5-year EFS and OS were 47% and 50%. NRM at day 100 and 5 years were 20% and 44%, respectively. Overall and CR rates on day 100 were 86% and 80%, respectively. The main causes of death were secondary to NRM: 32% GVHD, 32% infection, 3% veno-oclussive disease (VOD), 3% thrombotic microangiopathy and 15% others. Progression was the cause of death in only 14%. CI of relapse at 1 and 5 years were 9% and 16%, respectively. CI of grade 3-4 acute GVHD (aGVHD) at day 100 and moderate/severe chronic GVHD at 5 years were 29% and 42%, respectively. In the multivariate analysis we found the following independent factors: ECOG PS > 1 (HR 3.2; p=0.017) and donor mismatch (HR 2.2; p=0.007) for EFS; ECOG PS>1 (HR 3.1; p=0.018) and previous ASCT (HR 2.1; p=0.004) for OS; and grade 3-4 aGVHD (RR 7.1; p<0.001) for NRM.
Conclusion
Our data confirmed that allo-SCT may be a curative option in R/R MCL with low CI of relapse, although NRM is still high, mainly secondary to aGVHD. Results are better for fit patients, using HLA-identical donor (related or unrelated) and without previous ASCT. However, in the era of new immunotherapy and target drugs, allo-SCT should only be considered in selected patients failing these new approaches.
Keyword(s): Allogeneic stem cell transplant, Mantle cell lymphoma
Abstract: EP1231
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
MCL has been associated with poor prognosis, chemorefractoriness and older median age at diagnosis. For transplant-eligible patients, clinical outcome improves using intensive cytarabine-based induction, followed by autologous stem cell transplant (ASCT). Recently, new approaches with anti-CD20 maintenance, new target drugs or new ways of immunotherapy such as CARTs are changing the therapeutic landscape. Allo-SCT is a curative option for selected patients but with significant non-relapse mortality (NRM).
Aims
Our objective was to analyze long-term results in patients receiving allo-SCT in Spain.
Methods
We performed a retrospective multicenter study including patients from centers of GETH/GELTAMO with relapsed/refractory (R/R) MCL treated with allo-SCT from March 1995 to February 2020. The primary endpoints were event-free survival (EFS), overall survival (OS), NRM and cumulative incidence (CI) of relapse and graft versus host disease (GVHD).
Results
We included one-hundred and thirty-five patients with R/R MCL that fulfilled the inclusion criteria (Table 1). Median age was 56 years (27% >60 years); 49% had previous ASCT and median number of previous lines of therapy were 2 (1-8). Disease status at allo-SCT was complete response (CR) in 64%, partial response (PR) in 26% and stable/progressive disease (SD/PD) in 10%. Most patients (85%) received reduced intensity conditioning (RIC). After a median follow-up of 68 months (2-247), 5-year EFS and OS were 47% and 50%. NRM at day 100 and 5 years were 20% and 44%, respectively. Overall and CR rates on day 100 were 86% and 80%, respectively. The main causes of death were secondary to NRM: 32% GVHD, 32% infection, 3% veno-oclussive disease (VOD), 3% thrombotic microangiopathy and 15% others. Progression was the cause of death in only 14%. CI of relapse at 1 and 5 years were 9% and 16%, respectively. CI of grade 3-4 acute GVHD (aGVHD) at day 100 and moderate/severe chronic GVHD at 5 years were 29% and 42%, respectively. In the multivariate analysis we found the following independent factors: ECOG PS > 1 (HR 3.2; p=0.017) and donor mismatch (HR 2.2; p=0.007) for EFS; ECOG PS>1 (HR 3.1; p=0.018) and previous ASCT (HR 2.1; p=0.004) for OS; and grade 3-4 aGVHD (RR 7.1; p<0.001) for NRM.
Conclusion
Our data confirmed that allo-SCT may be a curative option in R/R MCL with low CI of relapse, although NRM is still high, mainly secondary to aGVHD. Results are better for fit patients, using HLA-identical donor (related or unrelated) and without previous ASCT. However, in the era of new immunotherapy and target drugs, allo-SCT should only be considered in selected patients failing these new approaches.
Keyword(s): Allogeneic stem cell transplant, Mantle cell lymphoma


