
Contributions
Abstract: EP1230
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Mixed phenotype acute leukemia (MPAL) is rare and generally associated with a poor prognosis. Optimal treatment for patients with MPAL and the role of allogeneic hematopoietic stem cell transplant (allo-SCT) remain unclear. Most prior case series included only modest numbers of transplanted patients, among which haploidentical transplant (haplo-SCT) were rarely included.
Aims
We tried to evaluate the safety and efficacy of haplo-SCT for MPAL patients and attempted to define factors that confer high-risk disease.
Methods
We retrospectively analyzed clinical results among MPAL diagnosed patients, defined by the 2017 World Health Organization (WHO) criteria. All patients included underwent a transplant at the Lu Daopei Hospital between July 2012 and December 2020. The latest follow-up date was December 2020.
Results
MPAL accounted for 3.1% (131 out of 4212) of all acute leukemias. Our analysis included the 111 MPAL patients who underwent unmanipulated haplo-HSCT with antithymocyte globulin [AA1] (ATG). Median age at transplant was 15 years (range: 1- 60 years of age). Patients had one of three immunophenotypes: 61 patients had leukemia with B/myeloid marker, 65 with T/myeloid marker, and 5 had B/T/myeloid markers. Fifteen patients harbored a BCR-ABL1 rearrangement and five had KMT2A-rearranged MPAL. Seventy-nine patients were in first complete remission (CR1), 31 in CR2 and 23 were in none remission (NR). Myeloablative regimens were used in all patients, among which 80 cases were body irradiation-based (TBI, 2Gy×5~6) and 41 busulfan-based (3.2 mg/kg/day×4). Cyclosporine, short-term methotrexate, and mycophenolate mofetil were used for graft versus host disease (GVHD) prophylaxis. Median total mononuclear cell count (MNC) and the infused CD34+ cell count was 9.0 ×108/kg (range: 3.94-19.13 ×108/kg) and 4.72 ×106/kg (range: 1.27-12.57×106/kg). Except for two patients transplanted in advanced status both of whom died of sepsis on Day 2, all patients received neutrophil engraftment at a median 14 days (range: 9-34 days) post-transplant[AA2] . One hundred and four patients achieved platelet engraftment at a median 13 days post-transplant (6-73 days). Up to the latest follow-up date, the median survival time was 34 months (range: 1 - 93 months). The 3-year relapse rate was 12.1% (95% CI 5.4%>18.8%) and the 3-year non-relapse mortality (NRM) rate was 20.7%
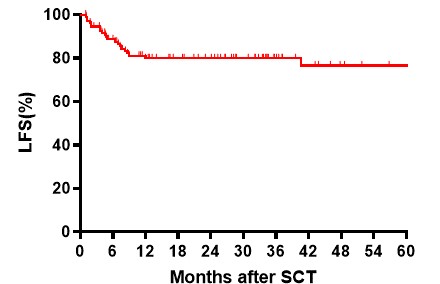
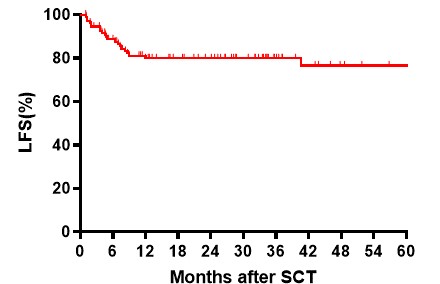
(95% CI 12.7-28.7%). The 3-year overall survival (OS) and 3-year leukemia-free survival (LFS) were 69.5% (95% CI 60.5-78.5%) and 69.6% (95% CI 60.8-78.4%), respectively. The 3-year LFS of patients in CR1 and ≥CR2 and those with advanced disease were 75.4% (95% CI 64.2-86.6%), 70.1% (95% CI 52.7-87.5%), and 52.5% (95% CI 31.1-73.9%), respectively (CR1vs.≥CR2 p=0.416; CR1 vs. advanced disease p=0.024; CR2 vs. advanced disease p=0.213). There were no differences in relapse rate, NRM, OS or LFS among patients in the three different immunophenotype groups (B/myeloid vs. T/myeloid), nor by age (<13 years vs. ≥14years), conditioning regimes (TBI-based vs. Bu-based), or date of transplant (2012-2017 vs. 2018-2020). In multivariate analyses, status before transplant was the only predictor of relapse rate (hazard ratio [HR] 2.151;95% CI, 1.058-4.375;p=0.034), OS (HR 1.598;95%CI, 1.048-2.435;p=0.033) and LFS (HR 1.574;95%CI, 1.044-2.375;p=0.031).
Conclusion
Haplo-SCT is a promising treatment option for patients with MPAL with encouraging low rates of relapse and long-term survival. Patients who undergo transplantation at an earlier stage of disease may have better safety and efficacy outcomes.
Keyword(s): Allogeneic hematopoietic stem cell transplant, Haploidentical stem cell transplantation, Mixed lineage leukemia, Survival
Abstract: EP1230
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Mixed phenotype acute leukemia (MPAL) is rare and generally associated with a poor prognosis. Optimal treatment for patients with MPAL and the role of allogeneic hematopoietic stem cell transplant (allo-SCT) remain unclear. Most prior case series included only modest numbers of transplanted patients, among which haploidentical transplant (haplo-SCT) were rarely included.
Aims
We tried to evaluate the safety and efficacy of haplo-SCT for MPAL patients and attempted to define factors that confer high-risk disease.
Methods
We retrospectively analyzed clinical results among MPAL diagnosed patients, defined by the 2017 World Health Organization (WHO) criteria. All patients included underwent a transplant at the Lu Daopei Hospital between July 2012 and December 2020. The latest follow-up date was December 2020.
Results
MPAL accounted for 3.1% (131 out of 4212) of all acute leukemias. Our analysis included the 111 MPAL patients who underwent unmanipulated haplo-HSCT with antithymocyte globulin [AA1] (ATG). Median age at transplant was 15 years (range: 1- 60 years of age). Patients had one of three immunophenotypes: 61 patients had leukemia with B/myeloid marker, 65 with T/myeloid marker, and 5 had B/T/myeloid markers. Fifteen patients harbored a BCR-ABL1 rearrangement and five had KMT2A-rearranged MPAL. Seventy-nine patients were in first complete remission (CR1), 31 in CR2 and 23 were in none remission (NR). Myeloablative regimens were used in all patients, among which 80 cases were body irradiation-based (TBI, 2Gy×5~6) and 41 busulfan-based (3.2 mg/kg/day×4). Cyclosporine, short-term methotrexate, and mycophenolate mofetil were used for graft versus host disease (GVHD) prophylaxis. Median total mononuclear cell count (MNC) and the infused CD34+ cell count was 9.0 ×108/kg (range: 3.94-19.13 ×108/kg) and 4.72 ×106/kg (range: 1.27-12.57×106/kg). Except for two patients transplanted in advanced status both of whom died of sepsis on Day 2, all patients received neutrophil engraftment at a median 14 days (range: 9-34 days) post-transplant[AA2] . One hundred and four patients achieved platelet engraftment at a median 13 days post-transplant (6-73 days). Up to the latest follow-up date, the median survival time was 34 months (range: 1 - 93 months). The 3-year relapse rate was 12.1% (95% CI 5.4%>18.8%) and the 3-year non-relapse mortality (NRM) rate was 20.7%
(95% CI 12.7-28.7%). The 3-year overall survival (OS) and 3-year leukemia-free survival (LFS) were 69.5% (95% CI 60.5-78.5%) and 69.6% (95% CI 60.8-78.4%), respectively. The 3-year LFS of patients in CR1 and ≥CR2 and those with advanced disease were 75.4% (95% CI 64.2-86.6%), 70.1% (95% CI 52.7-87.5%), and 52.5% (95% CI 31.1-73.9%), respectively (CR1vs.≥CR2 p=0.416; CR1 vs. advanced disease p=0.024; CR2 vs. advanced disease p=0.213). There were no differences in relapse rate, NRM, OS or LFS among patients in the three different immunophenotype groups (B/myeloid vs. T/myeloid), nor by age (<13 years vs. ≥14years), conditioning regimes (TBI-based vs. Bu-based), or date of transplant (2012-2017 vs. 2018-2020). In multivariate analyses, status before transplant was the only predictor of relapse rate (hazard ratio [HR] 2.151;95% CI, 1.058-4.375;p=0.034), OS (HR 1.598;95%CI, 1.048-2.435;p=0.033) and LFS (HR 1.574;95%CI, 1.044-2.375;p=0.031).
Conclusion
Haplo-SCT is a promising treatment option for patients with MPAL with encouraging low rates of relapse and long-term survival. Patients who undergo transplantation at an earlier stage of disease may have better safety and efficacy outcomes.
Keyword(s): Allogeneic hematopoietic stem cell transplant, Haploidentical stem cell transplantation, Mixed lineage leukemia, Survival


