
Contributions
Abstract: EP1203
Type: E-Poster Presentation
Session title: Sickle cell disease
Background
The mutation of the beta-globin gene that causes sickle cell disease (SCD), results in pleiotropic effects, such as haemolysis and vaso-occlusive crisis (VOC) that can induce inflammatory mechanisms with deleterious consequences on the organism. In fact, the activation of inflammatory cells (endothelial activation followed by a monocytic-neutrophilic response) and their intracellular pathways yield the production and secretion of numerous molecules that promote inflammation, including cytokines, chemokines, and growth factors. Few studies are currently available that evaluate the circulating levels of these molecules in a pediatric population.
Aims
The aim of this study is to identify a cytokine signature in a pediatric SCD population associated with specific clinical correlations.
Methods
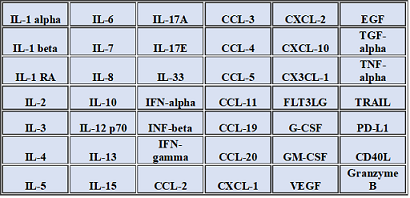
This study includes 35 patients with SCD (23 males and 12 females, medium age 9.3 years, range 0-20 years) at steady state (no current haemolytic crises or VOC or other acute complications) and 10 healthy controls matched for age and ethnicity. A panel of 42 serum cytokines was measured using Luminex Performance Human XL-Cytokine-Discovery-Magnetic-Panel following the manufacturers’ instructions (see table 1 for the list of analytes). These results were statistically related to clinical (age, gender, number of VOC per year, number of transfusions per year, pharmacological therapy) and laboratory data, such as hemoglobin (Hb)S, HbF and erythropoietin (EPO). Statistical analysis was performed to compare and correlate data. Data considered with statistical significance were those with p-value <0.05 and are therefore the ones presented in the results section.
Results
Significantly lower levels of IL-3, IL-4, IL-5, IL-7, IL-10, G-CSF and GM-CSF with higher levels of CXCL-2, CXCL-10, CCL-3, CCL-19 were observed in patients with SCD, compared to healthy donors. Furthermore, the group of patients who experienced VOC with higher frequency (1 or more crisis per year versus less than 1 crisis per year), showed lower levels of IL-3, IL-4 and IL-7. On the other hand, patients who underwent more frequently transfusion procedures (2 or more transfusions per year versus less than 2 transfusions per year) showed higher levels of IL-8, CCL-2, programmed death-ligand 1 (PD-L1), tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) and TGF-alpha. We also related cytokines levels to laboratory data, finding a direct correlation between HbS concentration, EGF and CXCL-2; an inverse relation was observed between HbF and CCL-2. Also, a positive correlation was found between EPO, IL-3 and PD-L1.
Conclusion
These results showed that our population of patients with SCD displayed higher levels of specific chemokines compared to HDs and lower levels of cytokines related to a Th2 response, cytokines involved in bone marrow omeostasis (IL-3 and IL-7) and growth factors, possibly related to bone marrow exhaustion. Moreover, we interestingly found that different phenotypes of patients displayed different signatures of cytokines: in particular patients who experienced more VOC showed lower levels of Th2 related cytokines with lower concentration of IL-3 and IL-7 as well; on the other hand, patients with greater transfusion needs, expressed higher levels of cytokines related to apoptosis control and specific chemokines, as CCL-2; coherently, we observed that increased concentrations of EPO are related to higher levels of PD-L1.
Keyword(s): Cytokine, Inflammation, Sickle cell anemia, Sickle cell disease
Abstract: EP1203
Type: E-Poster Presentation
Session title: Sickle cell disease
Background
The mutation of the beta-globin gene that causes sickle cell disease (SCD), results in pleiotropic effects, such as haemolysis and vaso-occlusive crisis (VOC) that can induce inflammatory mechanisms with deleterious consequences on the organism. In fact, the activation of inflammatory cells (endothelial activation followed by a monocytic-neutrophilic response) and their intracellular pathways yield the production and secretion of numerous molecules that promote inflammation, including cytokines, chemokines, and growth factors. Few studies are currently available that evaluate the circulating levels of these molecules in a pediatric population.
Aims
The aim of this study is to identify a cytokine signature in a pediatric SCD population associated with specific clinical correlations.
Methods
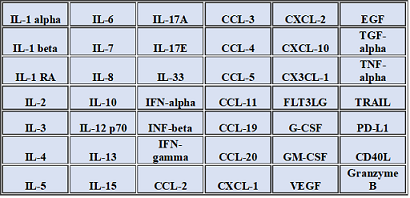
This study includes 35 patients with SCD (23 males and 12 females, medium age 9.3 years, range 0-20 years) at steady state (no current haemolytic crises or VOC or other acute complications) and 10 healthy controls matched for age and ethnicity. A panel of 42 serum cytokines was measured using Luminex Performance Human XL-Cytokine-Discovery-Magnetic-Panel following the manufacturers’ instructions (see table 1 for the list of analytes). These results were statistically related to clinical (age, gender, number of VOC per year, number of transfusions per year, pharmacological therapy) and laboratory data, such as hemoglobin (Hb)S, HbF and erythropoietin (EPO). Statistical analysis was performed to compare and correlate data. Data considered with statistical significance were those with p-value <0.05 and are therefore the ones presented in the results section.
Results
Significantly lower levels of IL-3, IL-4, IL-5, IL-7, IL-10, G-CSF and GM-CSF with higher levels of CXCL-2, CXCL-10, CCL-3, CCL-19 were observed in patients with SCD, compared to healthy donors. Furthermore, the group of patients who experienced VOC with higher frequency (1 or more crisis per year versus less than 1 crisis per year), showed lower levels of IL-3, IL-4 and IL-7. On the other hand, patients who underwent more frequently transfusion procedures (2 or more transfusions per year versus less than 2 transfusions per year) showed higher levels of IL-8, CCL-2, programmed death-ligand 1 (PD-L1), tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) and TGF-alpha. We also related cytokines levels to laboratory data, finding a direct correlation between HbS concentration, EGF and CXCL-2; an inverse relation was observed between HbF and CCL-2. Also, a positive correlation was found between EPO, IL-3 and PD-L1.
Conclusion
These results showed that our population of patients with SCD displayed higher levels of specific chemokines compared to HDs and lower levels of cytokines related to a Th2 response, cytokines involved in bone marrow omeostasis (IL-3 and IL-7) and growth factors, possibly related to bone marrow exhaustion. Moreover, we interestingly found that different phenotypes of patients displayed different signatures of cytokines: in particular patients who experienced more VOC showed lower levels of Th2 related cytokines with lower concentration of IL-3 and IL-7 as well; on the other hand, patients with greater transfusion needs, expressed higher levels of cytokines related to apoptosis control and specific chemokines, as CCL-2; coherently, we observed that increased concentrations of EPO are related to higher levels of PD-L1.
Keyword(s): Cytokine, Inflammation, Sickle cell anemia, Sickle cell disease


