
Contributions
Abstract: EP1189
Type: E-Poster Presentation
Session title: Quality of life, palliative care, ethics and health economics
Background
ASCT is standard of care in biologically fit, newly diagnosed MM (NDMM) patients (pts), offering deeper responses with prolonged progression free/overall survival and improved quality of life (QOL). However, with the UK’s 1st national lockdown on 23/03/2020, several guidelines recommended deferring ASCT for MM due to risks of infection, with resource limitations forcing some units to suspend ASCT entirely. Such changes to pts’ treatment plans inevitably altered their lived experience during these uncertain times with expected impact on QOL.
Aims
To provide a snapshot of how COVID-19 affected the MM ASCT service in a single UK institution, including changes to chemotherapy treatment plans, timing, and prioritisation of ASCT. To gain insight into MM pts’ understanding of their disease, initial therapy and ASCT, and their response to therapy changes.
Methods
We collected data on 115 NDMM pts who had a stem cell harvest (PBSCH) for upfront ASCT from December 2019–January 2021. During this time, 3 national lockdowns led to the ASCT service being suspended twice (March–June 2020 and January–February 2021). 25 pts within this cohort underwent a semi-structured interview via telephone. Inductive and deductive framework analysis was utilised to determine key themes and subthemes.
Results
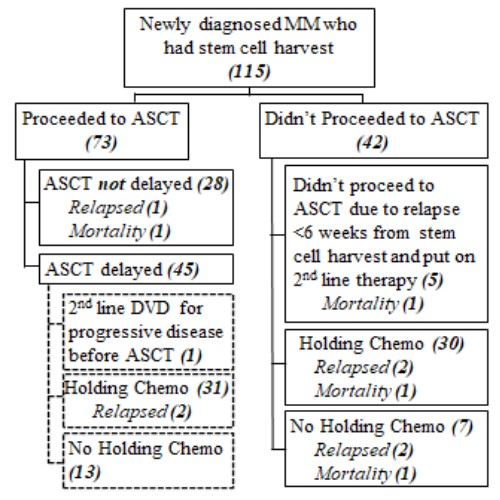
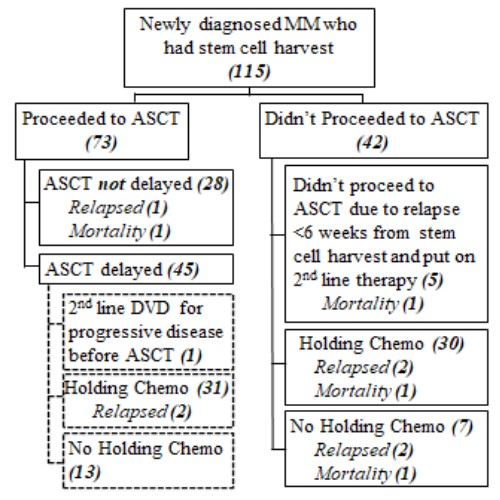
Pts were discussed in multidisciplinary meetings and decisions taken to delay or defer ASCT based on pt fitness, disease risk and depth of response. 73 (63%) proceeded to ASCT and 42 (37%) were deferred indefinitely (ASCTdef). The 2 groups were similar in terms of gender, age and ISS, but there were more pts with adverse risk cytogenetics in the ASCT group (26% vs 12%). Both groups were predominantly treated with bortezomib-based induction; in 11/73 (15%) ASCT and 7/42 (16.7%) ASCTdef pts treatment was changed to an oral, lenalidomide-based regimen to reduce hospital attendances for parenteral therapy. Overall response to induction in the 2 groups was similar; 97.3% and 95.2% and ³VGPR 59% and 52.4% in ASCT and ASCTdef pts respectively. 28/73 ASCT pts had no delay to ASCT and none received bridging chemotherapy; 45/73 had delayed ASCT (median 11 months [5–17] from start of induction) of whom 31 were put on bridging chemotherapy. In the 42 ASCTdef pts, 5 relapsed within ≤6 weeks of PBSCH and received 2nd line therapy, 30 were put on holding chemotherapy (previously not offered in the UK) as per NHS England COVID-19 interim guidance and 7 remained treatment-free post-induction.
Thematic analysis identified 6 overarching themes: a) psychological response to diagnosis and initial therapy, b) beliefs and opinions about the benefits of ASCT, c) perceptions of information provided about MM and ASCT, d) high levels of fear and anxiety around COVID-19 and e) feelings about ASCT disruption or delay due to COVID-19 f) perceptions of care. Example subthemes were beliefs that ASCT would provide a long-remission/best chance of normality including freedom from chemotherapy and associated side-effects, disappointment and devastation at COVID-related treatment delays (in spite of high anxiety about infection) and exceptionally high levels of trust in the transplant team.
Conclusion
New COVID-19-adapted guidelines, and new ways of perceiving and balancing risks of ASCT, led to a substantial proportion of MM pts having a delayed or indefinitely deferred ASCT. Such enforced changes gave us an opportunity to explore pts’ attitudes, perceptions, and expectations around MM and ASCT. Insights gained will help us adjust our service and counselling approaches to be more in tune with pts’ priorities and expectations.
Keyword(s): Autologous hematopoietic stem cell transplantation, COVID-19, Multiple myeloma, Quality of life
Abstract: EP1189
Type: E-Poster Presentation
Session title: Quality of life, palliative care, ethics and health economics
Background
ASCT is standard of care in biologically fit, newly diagnosed MM (NDMM) patients (pts), offering deeper responses with prolonged progression free/overall survival and improved quality of life (QOL). However, with the UK’s 1st national lockdown on 23/03/2020, several guidelines recommended deferring ASCT for MM due to risks of infection, with resource limitations forcing some units to suspend ASCT entirely. Such changes to pts’ treatment plans inevitably altered their lived experience during these uncertain times with expected impact on QOL.
Aims
To provide a snapshot of how COVID-19 affected the MM ASCT service in a single UK institution, including changes to chemotherapy treatment plans, timing, and prioritisation of ASCT. To gain insight into MM pts’ understanding of their disease, initial therapy and ASCT, and their response to therapy changes.
Methods
We collected data on 115 NDMM pts who had a stem cell harvest (PBSCH) for upfront ASCT from December 2019–January 2021. During this time, 3 national lockdowns led to the ASCT service being suspended twice (March–June 2020 and January–February 2021). 25 pts within this cohort underwent a semi-structured interview via telephone. Inductive and deductive framework analysis was utilised to determine key themes and subthemes.
Results
Pts were discussed in multidisciplinary meetings and decisions taken to delay or defer ASCT based on pt fitness, disease risk and depth of response. 73 (63%) proceeded to ASCT and 42 (37%) were deferred indefinitely (ASCTdef). The 2 groups were similar in terms of gender, age and ISS, but there were more pts with adverse risk cytogenetics in the ASCT group (26% vs 12%). Both groups were predominantly treated with bortezomib-based induction; in 11/73 (15%) ASCT and 7/42 (16.7%) ASCTdef pts treatment was changed to an oral, lenalidomide-based regimen to reduce hospital attendances for parenteral therapy. Overall response to induction in the 2 groups was similar; 97.3% and 95.2% and ³VGPR 59% and 52.4% in ASCT and ASCTdef pts respectively. 28/73 ASCT pts had no delay to ASCT and none received bridging chemotherapy; 45/73 had delayed ASCT (median 11 months [5–17] from start of induction) of whom 31 were put on bridging chemotherapy. In the 42 ASCTdef pts, 5 relapsed within ≤6 weeks of PBSCH and received 2nd line therapy, 30 were put on holding chemotherapy (previously not offered in the UK) as per NHS England COVID-19 interim guidance and 7 remained treatment-free post-induction.
Thematic analysis identified 6 overarching themes: a) psychological response to diagnosis and initial therapy, b) beliefs and opinions about the benefits of ASCT, c) perceptions of information provided about MM and ASCT, d) high levels of fear and anxiety around COVID-19 and e) feelings about ASCT disruption or delay due to COVID-19 f) perceptions of care. Example subthemes were beliefs that ASCT would provide a long-remission/best chance of normality including freedom from chemotherapy and associated side-effects, disappointment and devastation at COVID-related treatment delays (in spite of high anxiety about infection) and exceptionally high levels of trust in the transplant team.
Conclusion
New COVID-19-adapted guidelines, and new ways of perceiving and balancing risks of ASCT, led to a substantial proportion of MM pts having a delayed or indefinitely deferred ASCT. Such enforced changes gave us an opportunity to explore pts’ attitudes, perceptions, and expectations around MM and ASCT. Insights gained will help us adjust our service and counselling approaches to be more in tune with pts’ priorities and expectations.
Keyword(s): Autologous hematopoietic stem cell transplantation, COVID-19, Multiple myeloma, Quality of life


