
Contributions
Abstract: EP1188
Type: E-Poster Presentation
Session title: Quality of life, palliative care, ethics and health economics
Background
The outcome of patients with Hodgkin's lymphoma (HL) has greatly improved in recent years, which is why the attention of doctors and researchers has increasingly been diverted towards the well-being of these young patients. Consistent with this, the study aimed to analyze the influence of HL and its treatment on the fertility status of young males and detect new predictors affecting the likelihood of parenthood.
Aims
Consistent with this, the study aimed to analyze the influence of HL and its treatment on the fertility status of young males and detect new predictors affecting the likelihood of parenthood.
Methods
In this retrospective study, the fertility status of 42 male patients (mean age 25 years) with HL treated at the University Hospital of Bari (Italy) between 2008 and 2016 was studied. All were assessed for fertility at diagnosis, while 24 had post-treatment fertility status checks. All patients underwent ABVD as first-line chemotherapy, of them 6 patients with relapsed/ refractory disease underwent autologous hematopoietic stem cell transplantation (ASCT).
Results
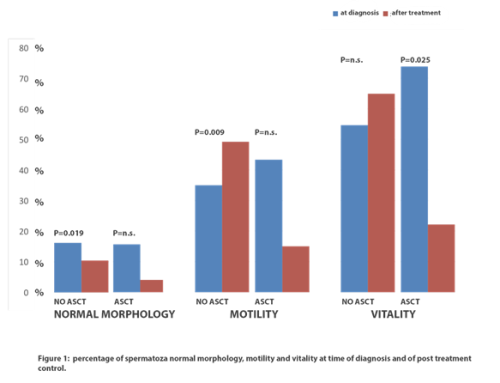
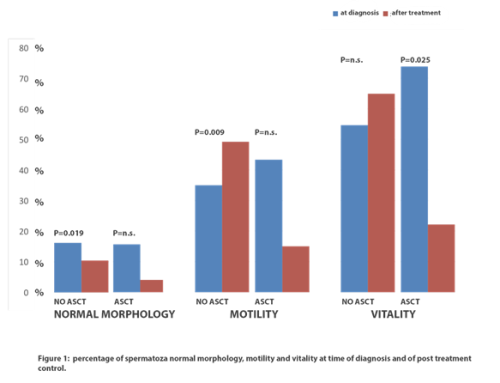
At the time of diagnosis, we found that 15 (35%) patients had normozoospermia, 19 (45%) oligozoospermia (of these 14 had other despermias), and 8 (19%) only other despermic conditions. After treatment, 17% of patients had azoospermia (all had undergone ASCT). Of the 9 normozoospermic patients at the time of diagnosis, 5 (55.5%) maintained that condition after treatment, while 4 (45.5%) developed azoospermia associated with other types of despermia (all undergoing ASCT). Of 11 patients with oligozoospermia and other types of despermia at the time of diagnosis treated with first line alone (no ASCT group), 6 (54%) normalized the fertility status after treatment; in the same group, 5 of 6 patients (83%) with normozoospermia at diagnosis maintained the status after treatment. Furthermore, in patients who received first-line treatment only, the mean sperm concentration was increased post-treatment (5.53 x10e7 at diagnosis vs 4.02 x10e7 after treatment).
We also found that 4/6 patients undergoing ASCT had azoospermia and despermia in the post-treatment control. On the other hand, 2 of the 3 patients, who had oligozoospermia before treatment, became normozoospermic after therapy. Furthermore, in univariate analysis, we found that patients undergoing ASCT were associated with severe impairment of fertility in terms of sperm motility (74% at diagnosis versus 22% after ASCT; p = 0.025, Fig. 1). In patients not undergoing ASCT we found a statistically significant improvement in fertility in terms of motility (35% at diagnosis versus 50% after treatment; p = 0.009, fig. 1)
Conclusion
In this study we found that ASCT induces infertility in the majority of male patients with HL and that first-line treatment could improve the fertility status caused by the disease. Further studies are needed in a larger case series to investigate risk factors for impaired fertility at diagnosis and after treatment.
Keyword(s):
Abstract: EP1188
Type: E-Poster Presentation
Session title: Quality of life, palliative care, ethics and health economics
Background
The outcome of patients with Hodgkin's lymphoma (HL) has greatly improved in recent years, which is why the attention of doctors and researchers has increasingly been diverted towards the well-being of these young patients. Consistent with this, the study aimed to analyze the influence of HL and its treatment on the fertility status of young males and detect new predictors affecting the likelihood of parenthood.
Aims
Consistent with this, the study aimed to analyze the influence of HL and its treatment on the fertility status of young males and detect new predictors affecting the likelihood of parenthood.
Methods
In this retrospective study, the fertility status of 42 male patients (mean age 25 years) with HL treated at the University Hospital of Bari (Italy) between 2008 and 2016 was studied. All were assessed for fertility at diagnosis, while 24 had post-treatment fertility status checks. All patients underwent ABVD as first-line chemotherapy, of them 6 patients with relapsed/ refractory disease underwent autologous hematopoietic stem cell transplantation (ASCT).
Results
At the time of diagnosis, we found that 15 (35%) patients had normozoospermia, 19 (45%) oligozoospermia (of these 14 had other despermias), and 8 (19%) only other despermic conditions. After treatment, 17% of patients had azoospermia (all had undergone ASCT). Of the 9 normozoospermic patients at the time of diagnosis, 5 (55.5%) maintained that condition after treatment, while 4 (45.5%) developed azoospermia associated with other types of despermia (all undergoing ASCT). Of 11 patients with oligozoospermia and other types of despermia at the time of diagnosis treated with first line alone (no ASCT group), 6 (54%) normalized the fertility status after treatment; in the same group, 5 of 6 patients (83%) with normozoospermia at diagnosis maintained the status after treatment. Furthermore, in patients who received first-line treatment only, the mean sperm concentration was increased post-treatment (5.53 x10e7 at diagnosis vs 4.02 x10e7 after treatment).
We also found that 4/6 patients undergoing ASCT had azoospermia and despermia in the post-treatment control. On the other hand, 2 of the 3 patients, who had oligozoospermia before treatment, became normozoospermic after therapy. Furthermore, in univariate analysis, we found that patients undergoing ASCT were associated with severe impairment of fertility in terms of sperm motility (74% at diagnosis versus 22% after ASCT; p = 0.025, Fig. 1). In patients not undergoing ASCT we found a statistically significant improvement in fertility in terms of motility (35% at diagnosis versus 50% after treatment; p = 0.009, fig. 1)
Conclusion
In this study we found that ASCT induces infertility in the majority of male patients with HL and that first-line treatment could improve the fertility status caused by the disease. Further studies are needed in a larger case series to investigate risk factors for impaired fertility at diagnosis and after treatment.
Keyword(s):


