
Contributions
Abstract: EP1168
Type: E-Poster Presentation
Session title: Quality of life, palliative care, ethics and health economics
Background
COVID-19 fatality can be as high as 30% in patients with hematological malignancies and hematopoietic stem cell transplant (HSCT) recipients.
Hospital-at-home (HAH) programs have significantly spread out in the last years and have demonstrated to improve patients satisfaction, avoid unnecessary hospital admissions and reduce healthcare costs.
Aims
To describe the implementation of an HAH unit for patients with hematological malignancies and HSCT recipients during the COVID-19 pandemic.
Methods
We retrospectively analysed the implementation of an HAH unit for caring hematological patients in our centre. In January 2020, we started our HAH unit, initially created for specific programs: at-home autologous HSCT for patients with multiple myeloma (MM), at-home consolidation treatment for patients with acute leukemia and intravenous treatment delivery. During March and April, simultaneously with the highest peak of the pandemic, the program expanded to other areas as part of our department strategy to ensure safe and high quality care for our patients. Besides, prevention measures were adopted to avoid cross-infection between patients and nurses.
At-home episode was defined as any time a patient was included in the HAH unit for a specific program previously described until patient was discharged.
Results
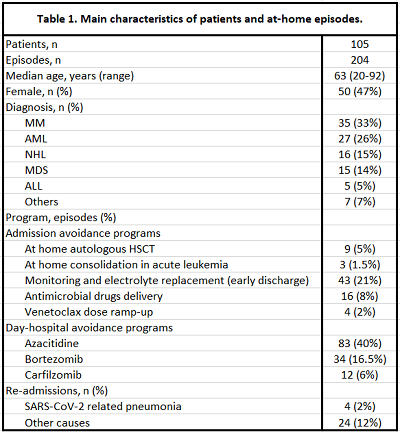
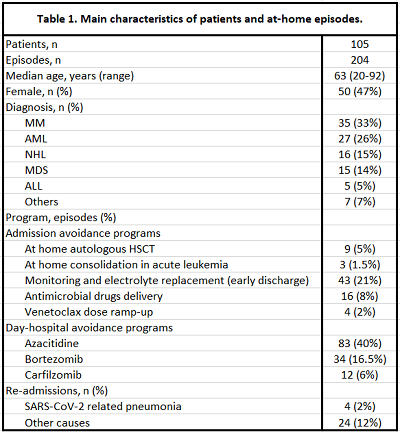
One hundred and five patients were included in the HAH unit between January 2020 and November 2020, with a total of 204 at-home episodes (Table 1). Nine at-home autologous HSCT were performed in 8 patients with MM (1 patient received a tandem transplant). All patients were discharged the day after infusion, except one with persistent vomiting, later discharged on day +5. Engraftment was achieved in a median time of 17 days (range 14-29) after transplant. Febrile neutropenia and engraftment syndrome rate was 0%.
Three patients were included in the at-home consolidation treatment program: 2 patients with AML and 1 with high-risk acute promyelocytic leukemia (APL). They were discharged from the hematology ward the day after cytarabine was fully administered.
Clinical and analytical monitoring or electrolyte replacement was performed at home in 32 patients (43 episodes). Five of these patients were autologous recipients who were discharged from HSCT unit before achieving engraftment, 15 were allogeneic HSCT recipients and 2 had received CAR-T cells therapy.
Azacitidine was administered at home to 22 patients (83 episodes), bortezomib to 22 patients (34 episodes) and carfilzomib to 8 patients (12 episodes).
Other episodes are described in Table 1.
Overall, more than 1000 visits were made to patients homes by nurses from the HAH unit, a median of 17 (IQR 13-19) days of admission per patient and a total of 239 visits to the hematology day-care hospital were avoided.
In summary, 28 patients (14% of all episodes) needed admission to the hospital while being treated by HAH unit, 4 of them because of SARS-CoV-2 related pneumonia. None of the nurses from the HAH unit developed SARS-CoV-2 infection while being actively caring patients at home, thus cross-transmission was discarded.
Conclusion
Implementation of a hematology HAH unit was feasible, safe and provided a thorough advanced care to a high risk population. Admissions and visits to day hospital were significantly reduced and SARS-CoV-2 infection rate was low and probably not related to cross-transmission between patients and nurses from the unit. In our experience, the use of advanced care at-home resulted crucial during times of COVID-19 to minimize treatment interruptions and reduce the risk of cross-infections.
Keyword(s): COVID-19, Hematological malignancy
Abstract: EP1168
Type: E-Poster Presentation
Session title: Quality of life, palliative care, ethics and health economics
Background
COVID-19 fatality can be as high as 30% in patients with hematological malignancies and hematopoietic stem cell transplant (HSCT) recipients.
Hospital-at-home (HAH) programs have significantly spread out in the last years and have demonstrated to improve patients satisfaction, avoid unnecessary hospital admissions and reduce healthcare costs.
Aims
To describe the implementation of an HAH unit for patients with hematological malignancies and HSCT recipients during the COVID-19 pandemic.
Methods
We retrospectively analysed the implementation of an HAH unit for caring hematological patients in our centre. In January 2020, we started our HAH unit, initially created for specific programs: at-home autologous HSCT for patients with multiple myeloma (MM), at-home consolidation treatment for patients with acute leukemia and intravenous treatment delivery. During March and April, simultaneously with the highest peak of the pandemic, the program expanded to other areas as part of our department strategy to ensure safe and high quality care for our patients. Besides, prevention measures were adopted to avoid cross-infection between patients and nurses.
At-home episode was defined as any time a patient was included in the HAH unit for a specific program previously described until patient was discharged.
Results
One hundred and five patients were included in the HAH unit between January 2020 and November 2020, with a total of 204 at-home episodes (Table 1). Nine at-home autologous HSCT were performed in 8 patients with MM (1 patient received a tandem transplant). All patients were discharged the day after infusion, except one with persistent vomiting, later discharged on day +5. Engraftment was achieved in a median time of 17 days (range 14-29) after transplant. Febrile neutropenia and engraftment syndrome rate was 0%.
Three patients were included in the at-home consolidation treatment program: 2 patients with AML and 1 with high-risk acute promyelocytic leukemia (APL). They were discharged from the hematology ward the day after cytarabine was fully administered.
Clinical and analytical monitoring or electrolyte replacement was performed at home in 32 patients (43 episodes). Five of these patients were autologous recipients who were discharged from HSCT unit before achieving engraftment, 15 were allogeneic HSCT recipients and 2 had received CAR-T cells therapy.
Azacitidine was administered at home to 22 patients (83 episodes), bortezomib to 22 patients (34 episodes) and carfilzomib to 8 patients (12 episodes).
Other episodes are described in Table 1.
Overall, more than 1000 visits were made to patients homes by nurses from the HAH unit, a median of 17 (IQR 13-19) days of admission per patient and a total of 239 visits to the hematology day-care hospital were avoided.
In summary, 28 patients (14% of all episodes) needed admission to the hospital while being treated by HAH unit, 4 of them because of SARS-CoV-2 related pneumonia. None of the nurses from the HAH unit developed SARS-CoV-2 infection while being actively caring patients at home, thus cross-transmission was discarded.
Conclusion
Implementation of a hematology HAH unit was feasible, safe and provided a thorough advanced care to a high risk population. Admissions and visits to day hospital were significantly reduced and SARS-CoV-2 infection rate was low and probably not related to cross-transmission between patients and nurses from the unit. In our experience, the use of advanced care at-home resulted crucial during times of COVID-19 to minimize treatment interruptions and reduce the risk of cross-infections.
Keyword(s): COVID-19, Hematological malignancy


