
Contributions
Abstract: EP1164
Type: E-Poster Presentation
Session title: Quality of life, palliative care, ethics and health economics
Background
A study in 2009 demonstrated there were a number of preventable serious incidents occurring in hospitals around the UK. These were termed Never Events(NE). In 2015, as a way to mitigate these serious incidents, the National Patient Safety Agency(NPSA) released a report, recommending the creation and implementation of National Safety Standards for Invasive Procedures(NatSSIPs), which at a local level would be named Local Safety Standards for Invasive Procedures(LocSSIPs). In 2017, University Hospitals Birmingham(UHB) NHS Foundation Trust set up a LocSSIP steering committee, with the commitment to create and implement LocSSIPs across the trust.
Aims
Our aim was to create and develop LocSSIPs within the haematology department and audit its implementation.
Methods
The project plan was divided into 4 phases: scoping, development, implementation and maintenance and monitoring. We identified a LocSSIP ‘champion’ within haematology and identified key procedures which would require LocSSIPs. Our safety standards were framed on NPSA guidance and standards of the WHO checklist but tailored for procedures within haematology. Following implementation, compliance was audited.
Results
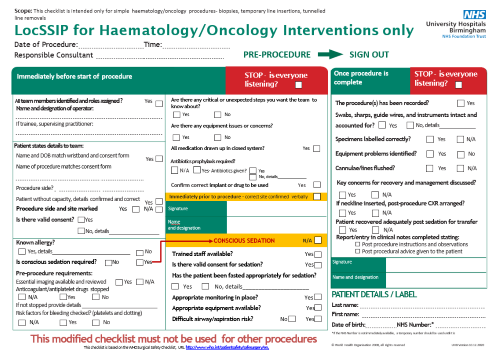
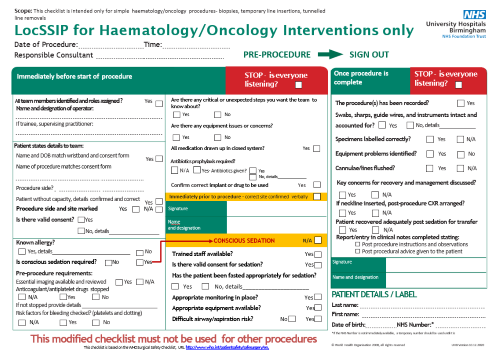
The LocSSIP checklist was successfully developed and approved for implementation. Pre-procedure and sign-out sections were created to allow safety checks before and after the procedures whilst allowing for efficiency and effective use. All questions were tailored to haematology such as bone marrow biopsies, lumbar punctures, and line insertions. Additionally, key safety questions for conscious sedation were created in line with local Trust and NICE guidance. Compliance of haematology LocSSIPs was 93.5% involving 31 procedures.
Informal feedback overall mentioned that staff members felt safer using LocSSIPs. Standardisation further facilitated patient safety following redeployment of staff due to the pandemic and recent merger of Trusts.
Conclusion
We have successfully demonstrated implementation and compliance of a LocSSIP in haematology. As with every quality improvement project, the work is longitudinal and the troubleshooting process is still ongoing. Continuous auditing and monitoring of their use is required as well as the long term effects on serious incidents.
Keyword(s): Patient, Safety
Abstract: EP1164
Type: E-Poster Presentation
Session title: Quality of life, palliative care, ethics and health economics
Background
A study in 2009 demonstrated there were a number of preventable serious incidents occurring in hospitals around the UK. These were termed Never Events(NE). In 2015, as a way to mitigate these serious incidents, the National Patient Safety Agency(NPSA) released a report, recommending the creation and implementation of National Safety Standards for Invasive Procedures(NatSSIPs), which at a local level would be named Local Safety Standards for Invasive Procedures(LocSSIPs). In 2017, University Hospitals Birmingham(UHB) NHS Foundation Trust set up a LocSSIP steering committee, with the commitment to create and implement LocSSIPs across the trust.
Aims
Our aim was to create and develop LocSSIPs within the haematology department and audit its implementation.
Methods
The project plan was divided into 4 phases: scoping, development, implementation and maintenance and monitoring. We identified a LocSSIP ‘champion’ within haematology and identified key procedures which would require LocSSIPs. Our safety standards were framed on NPSA guidance and standards of the WHO checklist but tailored for procedures within haematology. Following implementation, compliance was audited.
Results
The LocSSIP checklist was successfully developed and approved for implementation. Pre-procedure and sign-out sections were created to allow safety checks before and after the procedures whilst allowing for efficiency and effective use. All questions were tailored to haematology such as bone marrow biopsies, lumbar punctures, and line insertions. Additionally, key safety questions for conscious sedation were created in line with local Trust and NICE guidance. Compliance of haematology LocSSIPs was 93.5% involving 31 procedures.
Informal feedback overall mentioned that staff members felt safer using LocSSIPs. Standardisation further facilitated patient safety following redeployment of staff due to the pandemic and recent merger of Trusts.
Conclusion
We have successfully demonstrated implementation and compliance of a LocSSIP in haematology. As with every quality improvement project, the work is longitudinal and the troubleshooting process is still ongoing. Continuous auditing and monitoring of their use is required as well as the long term effects on serious incidents.
Keyword(s): Patient, Safety


