Contributions
Abstract: EP1158
Type: E-Poster Presentation
Session title: Platelet disorders
Background
Coeliac disease (CD) is often associated with other autoimmune disorders: the association with Immune Thrombocytopenia (ITP) has been investigated in some cohorts and case reports with contradictory results especially about gluten-free diet efficacy on ITP. No study aimed to describe the specific features of this association in pediatric age.
Aims
The aim of this study was to characterize the association of Cd and ITP in Italian children.
Methods
This is a multicenter retrospective study investigating the coexistence of CD and ITP in 28 children diagnosed from January 1th 2000 to December 31th 2019. A case report form was sent to all 55 A.I.E.O.P. Centers collecting information about patients up to 18 years of age with both CD and ITP. Informed consent was obtained from the parents or the legal guardians of all patients. CD was classified as classic (presence of symptoms of malabsorption, positive CD specific antibodies and biopsy, and symptoms resolution on a gluten-free diet), silent (positive CD specific antibodies, HLA DQ2 or DQ8 and biopsy without symptoms), latent (presence of HLA DQ2 or DQ8 and histological alterations typical of CD in duodenal biopsy at some point of their life, but neither symptoms nor positive antibodies) and potential (positive CD-specific antibodies and HLA without histological abnormalities in duodenal biopsies). ITP was defined as newly diagnosed (within 3 months from diagnosis), persistent (between 3 and 12 months from diagnosis) and chronic (cITP, lasting for more than 12 months). The ITP bleeding score was defined as Type A: asymptomatic-paucisymptomatic ITP, clinical symptoms ranging from no bleeding to few petechiae and some bruises without mucosal hemorrhages; type B: intermediate ITP, clinical picture with more petechiae, bruising and mucosal hemorrhages; type C: severe ITP, clinical picture with severe cutaneous and mucosal bleeding symptoms. As timing of diagnosis the patients were classified as CD first: CD was diagnosed before ITP; ITP first: ITP was diagnosed before CD; Simultaneous diagnosis: the second disease (CD or ITP) was diagnosed during hospitalization or initial ascertainment for the other disorder.
Results
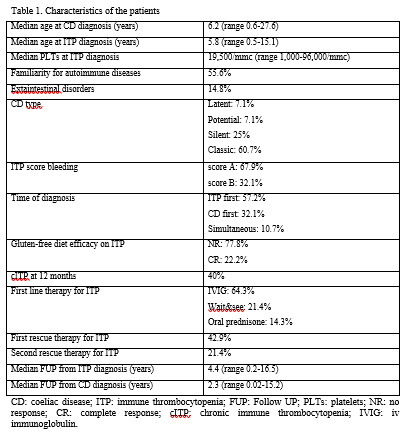
The most relevant clinical features of this cohort are shown in table I. The first diagnosis was ITP in 16 (57.2%) and CD in 9 patients (32.1%) respectively. In 3 patients (10.7%) the two diagnosis were simultaneous. The bleeding score of ITP was A in 67.9% and B in 32.1% of patients. ITP turned to be persistent in 44.4% and chronic in 40%. At the last FUP 28.6% of patients were still presenting cITP. The CD was classified as classical in 60.7% of children, silent in 25%, latent in 7.1% and potential in 7.1%. At ITP onset 21.4% of the patients were not treated (wait&see), 64.3% received iv immunoglobulin (IVIG) and 14.3% oral prednisone. Subsequent rescue therapies for ITP were attempted in 12 patients (42.9%). All the potential and silent CDs in our cohort were diagnosed in the 2 groups of ITP first or simultaneous diagnosis. In all children ITP was mild and in 2 out of 8 patients not recovered from ITP at the time of CD diagnosis a normalization of platelet counts (> 100,000/mmc) occurred after 3 and 5 months from starting gluten free diet.
Conclusion
We think that screening for celiac disease should be considered in children with ITP, regardless the presence of gastrointestinal symptoms. About one fourth of patients recover from ITP after starting gluten-free diet.
Keyword(s): Autoimmune disease, Children, ITP, Platelet
Abstract: EP1158
Type: E-Poster Presentation
Session title: Platelet disorders
Background
Coeliac disease (CD) is often associated with other autoimmune disorders: the association with Immune Thrombocytopenia (ITP) has been investigated in some cohorts and case reports with contradictory results especially about gluten-free diet efficacy on ITP. No study aimed to describe the specific features of this association in pediatric age.
Aims
The aim of this study was to characterize the association of Cd and ITP in Italian children.
Methods
This is a multicenter retrospective study investigating the coexistence of CD and ITP in 28 children diagnosed from January 1th 2000 to December 31th 2019. A case report form was sent to all 55 A.I.E.O.P. Centers collecting information about patients up to 18 years of age with both CD and ITP. Informed consent was obtained from the parents or the legal guardians of all patients. CD was classified as classic (presence of symptoms of malabsorption, positive CD specific antibodies and biopsy, and symptoms resolution on a gluten-free diet), silent (positive CD specific antibodies, HLA DQ2 or DQ8 and biopsy without symptoms), latent (presence of HLA DQ2 or DQ8 and histological alterations typical of CD in duodenal biopsy at some point of their life, but neither symptoms nor positive antibodies) and potential (positive CD-specific antibodies and HLA without histological abnormalities in duodenal biopsies). ITP was defined as newly diagnosed (within 3 months from diagnosis), persistent (between 3 and 12 months from diagnosis) and chronic (cITP, lasting for more than 12 months). The ITP bleeding score was defined as Type A: asymptomatic-paucisymptomatic ITP, clinical symptoms ranging from no bleeding to few petechiae and some bruises without mucosal hemorrhages; type B: intermediate ITP, clinical picture with more petechiae, bruising and mucosal hemorrhages; type C: severe ITP, clinical picture with severe cutaneous and mucosal bleeding symptoms. As timing of diagnosis the patients were classified as CD first: CD was diagnosed before ITP; ITP first: ITP was diagnosed before CD; Simultaneous diagnosis: the second disease (CD or ITP) was diagnosed during hospitalization or initial ascertainment for the other disorder.
Results
The most relevant clinical features of this cohort are shown in table I. The first diagnosis was ITP in 16 (57.2%) and CD in 9 patients (32.1%) respectively. In 3 patients (10.7%) the two diagnosis were simultaneous. The bleeding score of ITP was A in 67.9% and B in 32.1% of patients. ITP turned to be persistent in 44.4% and chronic in 40%. At the last FUP 28.6% of patients were still presenting cITP. The CD was classified as classical in 60.7% of children, silent in 25%, latent in 7.1% and potential in 7.1%. At ITP onset 21.4% of the patients were not treated (wait&see), 64.3% received iv immunoglobulin (IVIG) and 14.3% oral prednisone. Subsequent rescue therapies for ITP were attempted in 12 patients (42.9%). All the potential and silent CDs in our cohort were diagnosed in the 2 groups of ITP first or simultaneous diagnosis. In all children ITP was mild and in 2 out of 8 patients not recovered from ITP at the time of CD diagnosis a normalization of platelet counts (> 100,000/mmc) occurred after 3 and 5 months from starting gluten free diet.
Conclusion
We think that screening for celiac disease should be considered in children with ITP, regardless the presence of gastrointestinal symptoms. About one fourth of patients recover from ITP after starting gluten-free diet.
Keyword(s): Autoimmune disease, Children, ITP, Platelet