Contributions
Abstract: EP1155
Type: E-Poster Presentation
Session title: Platelet disorders
Background
Many extraintestinal autoimmune manifestations are reported in inflammatory bowel disease (IBD): Immune thrombocytopenia (ITP) can be associated: only a few patients are of pediatric age.
Aims
In this retrospective study we analyzed the largest series of children affected by both ITP and IBD. The coexistence of both diseases was investigated in children diagnosed from January 1th 2000 to December 31th 2019.
Methods
This retrospective study was designed by the Coagulation Defects Study Group of A.I.E.O.P. (Associazione Italiana Emato-Oncologia Pediatrica). Informed consent was obtained from the parents or the legal guardians of all patients. Clinical characteristics of both IBD and ITP, onset of disorders and patient’s response to treatment were collected through a structured form sent to 55 Italian pediatric referring centers for hematological disorders. IBDs were classified as Crohn disease (CD), Ulcerative colitis (UC) and Inflammatory bowel disease unclassified (IBDU). ITP was defined as newly diagnosed (within 3 months from diagnosis), persistent (between 3 and 12 months from diagnosis) and chronic (cITP, lasting for more than 12 months). The ITP bleeding score was defined as Type A: asymptomatic-paucisymptomatic ITP, clinical symptoms ranging from no bleeding to few petechiae and some bruises without mucosal hemorrhages; type B: intermediate ITP, clinical picture with more petechiae, bruising and mucosal hemorrhages; type C: severe ITP, clinical picture with severe cutaneous and mucosal bleeding symptoms. As timing of diagnosis the patients were classified as: 1) IBD first: IBD was diagnosed before ITP; 2) ITP first: ITP was diagnosed before IBD; 3) Simultaneous diagnosis: the second disease (IBD or ITP) was diagnosed during hospitalization or initial ascertainment for the other disorder.
Results
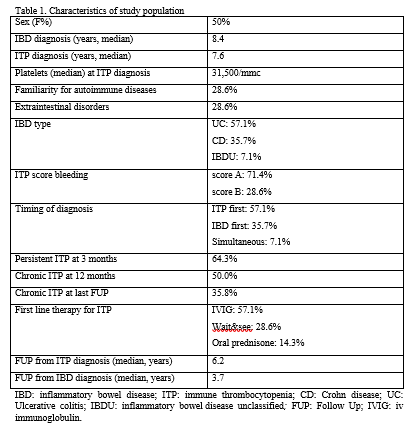
Centers responded to the survey and reported the coexistence of IBD and ITP in 14 children. The most relevant clinical features of this cohort are shown in table I. The first diagnosis was ITP in 57.1% and IBD in 35.7% of patients: it was simultaneous in 7.1%. IBD was classified as UC (57.1%), CD (35.7%) and IBDU (7.1%). The bleeding score was A in 71.4% and B in 28.6% of patients. ITP turned to be persistent in 9/14 patients (64.3%) and chronic in 7/14 (50%). At ITP onset 4/14 of the patients (28.6%) were not treated (wait&see), 8/14 (57.1%) received iv immunoglobulin (IVIG) and 2/14 (14.3%) oral prednisone. Subsequent rescue therapies for ITP were attempted in 7 patients (50.0%). At the last follow up 5/14 patients (35.8%) were still presenting cITP and 3 patients were still on treatment. No therapy for ITP other than steroids had any effect on IBD and vice versa. Colectomy resulted in recovery from ITP in 1 of the 2 patients surgically treated. At the last FUP 35.8% of patients were still presenting cITP and 3 patients were still on treatment (with eltrombopag).
Conclusion
We present the largest case series reported to date of children affected by both IBD and ITP. In all patients ITP was mild without any evident impact on IBD severity. It seems that UC is the type of IBD more commonly associated to ITP and that incidence of cITP (50%) is higher than what usually reported in pediatric age. Colectomy can occasionally result in ITP recovery and steroids can be effective in both diseases. Finally eltrombopag retains its high efficiency also in pediatric ITPs associated to IBD.
Keyword(s): Autoimmune disease, Children, Immune thrombocytopenia (ITP), Platelet
Abstract: EP1155
Type: E-Poster Presentation
Session title: Platelet disorders
Background
Many extraintestinal autoimmune manifestations are reported in inflammatory bowel disease (IBD): Immune thrombocytopenia (ITP) can be associated: only a few patients are of pediatric age.
Aims
In this retrospective study we analyzed the largest series of children affected by both ITP and IBD. The coexistence of both diseases was investigated in children diagnosed from January 1th 2000 to December 31th 2019.
Methods
This retrospective study was designed by the Coagulation Defects Study Group of A.I.E.O.P. (Associazione Italiana Emato-Oncologia Pediatrica). Informed consent was obtained from the parents or the legal guardians of all patients. Clinical characteristics of both IBD and ITP, onset of disorders and patient’s response to treatment were collected through a structured form sent to 55 Italian pediatric referring centers for hematological disorders. IBDs were classified as Crohn disease (CD), Ulcerative colitis (UC) and Inflammatory bowel disease unclassified (IBDU). ITP was defined as newly diagnosed (within 3 months from diagnosis), persistent (between 3 and 12 months from diagnosis) and chronic (cITP, lasting for more than 12 months). The ITP bleeding score was defined as Type A: asymptomatic-paucisymptomatic ITP, clinical symptoms ranging from no bleeding to few petechiae and some bruises without mucosal hemorrhages; type B: intermediate ITP, clinical picture with more petechiae, bruising and mucosal hemorrhages; type C: severe ITP, clinical picture with severe cutaneous and mucosal bleeding symptoms. As timing of diagnosis the patients were classified as: 1) IBD first: IBD was diagnosed before ITP; 2) ITP first: ITP was diagnosed before IBD; 3) Simultaneous diagnosis: the second disease (IBD or ITP) was diagnosed during hospitalization or initial ascertainment for the other disorder.
Results
Centers responded to the survey and reported the coexistence of IBD and ITP in 14 children. The most relevant clinical features of this cohort are shown in table I. The first diagnosis was ITP in 57.1% and IBD in 35.7% of patients: it was simultaneous in 7.1%. IBD was classified as UC (57.1%), CD (35.7%) and IBDU (7.1%). The bleeding score was A in 71.4% and B in 28.6% of patients. ITP turned to be persistent in 9/14 patients (64.3%) and chronic in 7/14 (50%). At ITP onset 4/14 of the patients (28.6%) were not treated (wait&see), 8/14 (57.1%) received iv immunoglobulin (IVIG) and 2/14 (14.3%) oral prednisone. Subsequent rescue therapies for ITP were attempted in 7 patients (50.0%). At the last follow up 5/14 patients (35.8%) were still presenting cITP and 3 patients were still on treatment. No therapy for ITP other than steroids had any effect on IBD and vice versa. Colectomy resulted in recovery from ITP in 1 of the 2 patients surgically treated. At the last FUP 35.8% of patients were still presenting cITP and 3 patients were still on treatment (with eltrombopag).
Conclusion
We present the largest case series reported to date of children affected by both IBD and ITP. In all patients ITP was mild without any evident impact on IBD severity. It seems that UC is the type of IBD more commonly associated to ITP and that incidence of cITP (50%) is higher than what usually reported in pediatric age. Colectomy can occasionally result in ITP recovery and steroids can be effective in both diseases. Finally eltrombopag retains its high efficiency also in pediatric ITPs associated to IBD.
Keyword(s): Autoimmune disease, Children, Immune thrombocytopenia (ITP), Platelet