
Contributions
Abstract: EP1135
Type: E-Poster Presentation
Session title: Platelet disorders
Background
Heparin induced thrombocytopenia (HIT) is characterised by a rapid fall in the platelet count normally 5-10 days after starting heparin therapy with or without thromboembolic complications and commonly seen in the cardiac population. For laboratory diagnosis of HIT antibodies, both antigen assays and platelet activation (functional) assays are available. Both tests are very sensitive (high negative predictive value) but specificity is problematic, especially for the antigen assays, which also detect non-pathogenic immunoglobulins. Functional tests including the Serotonin release assay (SRA) and heparin induced platelet activation (HIPA) are more specific but only available in specialised laboratories.
Aims
1. To assess the laboratory diagnosis for detecting anti-PF4/heparin antibodies and assays in cardiopulmonary bypass (CPB) cardio thoracic intensive care unit (ICU) patients. 2.To evaluates the positive and negative predictive value of various HIT laboratory tests and assess any correlation between HIT, the underlying diagnosis, underlying procedure, valve replacement and cardiac devices.
Methods
This is a retrospective 1-year study in CPB patients from a single cardiothoracic ICU centre. The ‘4 T’s’ (Thrombocytopenia, Timing of platelet count fall, Thrombosis and exclude other causes for Thrombocytopenia,) was used for the clinical diagnosis of HIT. Two laboratory diagnostic tests were performed, the pan specific screening test which includes pan specific antibodies IgG, IgA and IgM, followed by confirmatory HIT specific IgG ELISA. Functional assays, the SRA and HIPA were not available in our laboratories. Clinical details were obtained from ICU-ICCA7* system.
Results
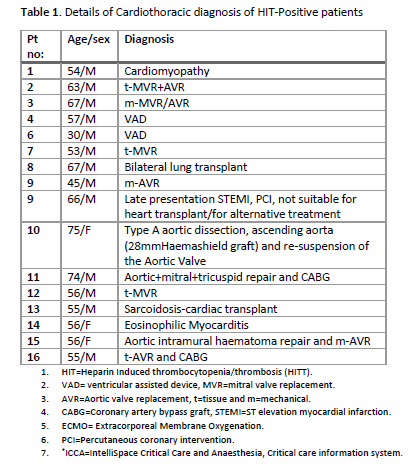
Total N=80 patients (F:23, M:57) had HIT probability “4 T” score >4. Total N=38 patients (48%) were HiT screen pan specific IgGAM negative and n=40 (50%) were HIT pan specific positive. Only n=14 patients (17%) were panspecific and HIT IgG ELISA positive and 2 cases were inconclusive. All HIT positive acute patients received Argatroban except one who received Fondaparinux. There were 5 unusual cases. One patient had Eosinophilic myocarditis and was HIT ELISA IgG neg but the 4-T score was >6 and patient received Argatroban and responded with platelet recovery and no further thrombosis. One patient with Sarcoidosis had aggressive course and received IV IG but succumbed secondary to bleeding. One patient progressed to gut ischemia and had surgical intervention but perished. Two patients with mechanical valves were on Argatroban/Warfarin but relapsed during ICU stepdown stage and received and responded to IV immunoglobulin. It is observed that 9/16 (>50%) HIT+patients had valve replacement or cardiac devices.
Conclusion
1. 80% of thrombocytopenia in ICU patients was secondary and not HIT related. 2. Pan specific HIT antibody test had positive predictive value of only 35% and Argatroban treatment based on pan specific antibody positivity may be uncertain and may lead to complications. 3.The autoimmune diseases patients like sarcoidosis and eosinophilic myocardits course varies in pathogenic and non-pathogenic HIT antibody production and clinical severity. The functional assays SRA or HIPA would be more useful in these cases. 4. Patients underlying diagnosis as well as underlying surgical procedures do play a key role in the incidence and severity of HIT and thrombosis 5. It may simply be a selected patients caseload surgery practice or an indication that patients with valve replacement and cardiac devices showed relatively higher HIT incidence and this requires larger studies and further investigations.
Keyword(s): Heparin induced thrombocytopenia (HIT), Thrombocytopenia, Thromboembolic events
Abstract: EP1135
Type: E-Poster Presentation
Session title: Platelet disorders
Background
Heparin induced thrombocytopenia (HIT) is characterised by a rapid fall in the platelet count normally 5-10 days after starting heparin therapy with or without thromboembolic complications and commonly seen in the cardiac population. For laboratory diagnosis of HIT antibodies, both antigen assays and platelet activation (functional) assays are available. Both tests are very sensitive (high negative predictive value) but specificity is problematic, especially for the antigen assays, which also detect non-pathogenic immunoglobulins. Functional tests including the Serotonin release assay (SRA) and heparin induced platelet activation (HIPA) are more specific but only available in specialised laboratories.
Aims
1. To assess the laboratory diagnosis for detecting anti-PF4/heparin antibodies and assays in cardiopulmonary bypass (CPB) cardio thoracic intensive care unit (ICU) patients. 2.To evaluates the positive and negative predictive value of various HIT laboratory tests and assess any correlation between HIT, the underlying diagnosis, underlying procedure, valve replacement and cardiac devices.
Methods
This is a retrospective 1-year study in CPB patients from a single cardiothoracic ICU centre. The ‘4 T’s’ (Thrombocytopenia, Timing of platelet count fall, Thrombosis and exclude other causes for Thrombocytopenia,) was used for the clinical diagnosis of HIT. Two laboratory diagnostic tests were performed, the pan specific screening test which includes pan specific antibodies IgG, IgA and IgM, followed by confirmatory HIT specific IgG ELISA. Functional assays, the SRA and HIPA were not available in our laboratories. Clinical details were obtained from ICU-ICCA7* system.
Results
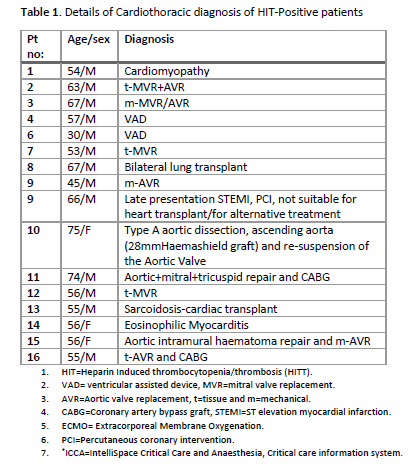
Total N=80 patients (F:23, M:57) had HIT probability “4 T” score >4. Total N=38 patients (48%) were HiT screen pan specific IgGAM negative and n=40 (50%) were HIT pan specific positive. Only n=14 patients (17%) were panspecific and HIT IgG ELISA positive and 2 cases were inconclusive. All HIT positive acute patients received Argatroban except one who received Fondaparinux. There were 5 unusual cases. One patient had Eosinophilic myocarditis and was HIT ELISA IgG neg but the 4-T score was >6 and patient received Argatroban and responded with platelet recovery and no further thrombosis. One patient with Sarcoidosis had aggressive course and received IV IG but succumbed secondary to bleeding. One patient progressed to gut ischemia and had surgical intervention but perished. Two patients with mechanical valves were on Argatroban/Warfarin but relapsed during ICU stepdown stage and received and responded to IV immunoglobulin. It is observed that 9/16 (>50%) HIT+patients had valve replacement or cardiac devices.
Conclusion
1. 80% of thrombocytopenia in ICU patients was secondary and not HIT related. 2. Pan specific HIT antibody test had positive predictive value of only 35% and Argatroban treatment based on pan specific antibody positivity may be uncertain and may lead to complications. 3.The autoimmune diseases patients like sarcoidosis and eosinophilic myocardits course varies in pathogenic and non-pathogenic HIT antibody production and clinical severity. The functional assays SRA or HIPA would be more useful in these cases. 4. Patients underlying diagnosis as well as underlying surgical procedures do play a key role in the incidence and severity of HIT and thrombosis 5. It may simply be a selected patients caseload surgery practice or an indication that patients with valve replacement and cardiac devices showed relatively higher HIT incidence and this requires larger studies and further investigations.
Keyword(s): Heparin induced thrombocytopenia (HIT), Thrombocytopenia, Thromboembolic events


