
Contributions
Abstract: EP1132
Type: E-Poster Presentation
Session title: Platelet disorders
Background
Misdiagnosed thrombocytopenia, mainly autoimmune forms, could lead to inadequate treatments with eventual development of side effects. Recently, the knowledge about inherited thrombocytopenia has expanded offering a new field of research and a new diagnostic, prognostic and therapeutic approach for these patients.
Aims
To evaluate the applicability and utility of a next generation sequencing (NGS) based gene panel in the diagnostic of suspected inherited thrombocytopenia in the clinical practice.
Methods
This prospective descriptive study included patients with a previous diagnosis of not specified thrombocytopenia who fulfilled inclusion criteria: not acquired thrombocytopenia (no previous normal range platelets count) and not known secondary causes of thrombocytopenia. A family history of thrombocytopenia and lack of response to immunosuppressive treatment were also recorded.
All participants underwent a complete medical and family history, a physical examination and several laboratory tests including a complete blood count, blood chemistry and a peripheral blood smear. A total of 200 platelets were evaluated in every blood smear and platelet size, granulation and vacuolization were described. Platelets larger than half a red blood cell were considered large forms. Bone marrow was recorded if it was previously studied. The NGS gene panel was performed to all the patients. Data are presented as medians, maximum, minimum and percentages. Informed consents were required for all patients.
Results
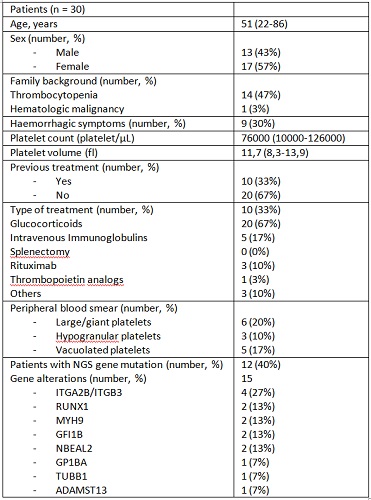
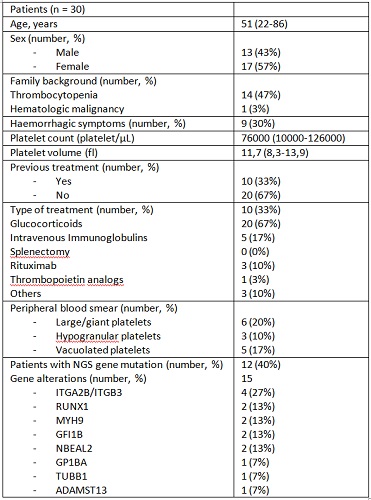
Thirty patients were included in the study. They were 51 (22-86) year old by median and showed a median platelet count of 76000/µl (10000 to 120000) and a median platelet volume of 11.7fl (8.3-13.9) at the time of the inclusion. Almost half of subjects (47%) had family history of thrombocytopenia and only 1 patients (3%) had family history of hematologic malignancy: one brother with an unknown type of acute leukaemia. None of the patients presented known syndromic disorder. Nine patients (30%) referred previous haemorrhagic complications, in most cases with mild symptoms. Ten (33%) participants received previous treatment for immune thrombocytopenia without response. Six (20%), 3 (10%) and 5 (17%) of the peripheral blood smear samples showed large, hypogranular and vacuolated platelets respectively. The NGS panel proved that 12 out of the 30 patients (40%) presented some genetic mutation related to inherited thrombocytopenia (see table 1). In total, 15 gene alterations were identified. It is remarkable that all the patients who showed large platelets in blood smear matched with some type of gene mutation.
Conclusion
In this one center experience, the application of a NGS based gene panel allowed to diagnose a considerable amount of patients with suspected inherited thrombocytopenia. Identifying these patients is important to avoid useless treatments (up 33% in our series) and to recognize some forms that can develop secondary diseases requiring follow-up in clinical practice.
Keyword(s): Inherited platelet disorders
Abstract: EP1132
Type: E-Poster Presentation
Session title: Platelet disorders
Background
Misdiagnosed thrombocytopenia, mainly autoimmune forms, could lead to inadequate treatments with eventual development of side effects. Recently, the knowledge about inherited thrombocytopenia has expanded offering a new field of research and a new diagnostic, prognostic and therapeutic approach for these patients.
Aims
To evaluate the applicability and utility of a next generation sequencing (NGS) based gene panel in the diagnostic of suspected inherited thrombocytopenia in the clinical practice.
Methods
This prospective descriptive study included patients with a previous diagnosis of not specified thrombocytopenia who fulfilled inclusion criteria: not acquired thrombocytopenia (no previous normal range platelets count) and not known secondary causes of thrombocytopenia. A family history of thrombocytopenia and lack of response to immunosuppressive treatment were also recorded.
All participants underwent a complete medical and family history, a physical examination and several laboratory tests including a complete blood count, blood chemistry and a peripheral blood smear. A total of 200 platelets were evaluated in every blood smear and platelet size, granulation and vacuolization were described. Platelets larger than half a red blood cell were considered large forms. Bone marrow was recorded if it was previously studied. The NGS gene panel was performed to all the patients. Data are presented as medians, maximum, minimum and percentages. Informed consents were required for all patients.
Results
Thirty patients were included in the study. They were 51 (22-86) year old by median and showed a median platelet count of 76000/µl (10000 to 120000) and a median platelet volume of 11.7fl (8.3-13.9) at the time of the inclusion. Almost half of subjects (47%) had family history of thrombocytopenia and only 1 patients (3%) had family history of hematologic malignancy: one brother with an unknown type of acute leukaemia. None of the patients presented known syndromic disorder. Nine patients (30%) referred previous haemorrhagic complications, in most cases with mild symptoms. Ten (33%) participants received previous treatment for immune thrombocytopenia without response. Six (20%), 3 (10%) and 5 (17%) of the peripheral blood smear samples showed large, hypogranular and vacuolated platelets respectively. The NGS panel proved that 12 out of the 30 patients (40%) presented some genetic mutation related to inherited thrombocytopenia (see table 1). In total, 15 gene alterations were identified. It is remarkable that all the patients who showed large platelets in blood smear matched with some type of gene mutation.
Conclusion
In this one center experience, the application of a NGS based gene panel allowed to diagnose a considerable amount of patients with suspected inherited thrombocytopenia. Identifying these patients is important to avoid useless treatments (up 33% in our series) and to recognize some forms that can develop secondary diseases requiring follow-up in clinical practice.
Keyword(s): Inherited platelet disorders


