
Contributions
Abstract: EP1118
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
Major thrombotic events are devastating complications in the Philadelphia negative myeloproliferative diseases. The neutrophil- lymphocyte ratio (NLR) and the platelet- lymphocyte ratio (PLR) were found to be associated with the burden of thrombotic events.
Aims
Our objective is to determine the role of NLR, and PLR ratios detected at the diagnosis of the MPN diseases as an indicator to thrombosis in conjugation with the other risk factors and to illustrate the difference between the patients developed thrombosis at the diagnosis of MPN disease and patients who develop the thrombosis after the diagnosis.
Methods
The current study is a single-center observational prospective cohort (NCT03599700, Clinical Trials.gov) conducted in a university-affiliated hospital (Assiut University Hospital, Assiut, Egypt).
Subjects were enrolled if BCR-ABL negative myeloproliferative neoplasms e.g.: Polycythemia vera, Essential thrombocythemia, and Primary myelofibrosis and the age was more than 18 years.
Clinical and demographic data were collected. Laboratory assessment included complete blood count (CBC). Follow up for thrombotic events were planned for three years from the start of the study. The patients were divided to three groups according to the incidence of thrombosis either no thrombosis or thrombosis at diagnosis of the MPN or thrombosis after the diagnosis of the disease.
Results
Within 15 months of the study, we recruited 204 patients with 142 patients (69.6%) of whom showed no thrombosis and 42 patients (20.6%) of the patients affected by thrombosis at the diagnosis and 20 patients (9.8%) of the patients developed thrombosis during their follow up.
We found that thrombosis at and after diagnosis occurred in 42 patients (27%) at age <65 years while it occurred in 20 patients (40.8%) at age ≥ 65 years group (P=0.05).
PLR showed a significant difference between Patients without thrombosis group and both Patients with thrombosis at diagnosis and after diagnosis groups (P= 0.002).
NLR showed a significant difference between Patients without thrombosis group and the group of Patients with thrombosis at diagnosis and after diagnosis groups (P= 0.03).
Univariate analysis was done for the thrombosis risk factors: sex, BMI, diagnosis subclassification, presence of constitutional symptoms, JAK mutation, PLR, NLR, age ≥65 years and smoking status.
PLR, constitutional symptoms, smoking status, JAK mutation and MPN subclassification were the significant factors and incorporated into multivariate analysis.
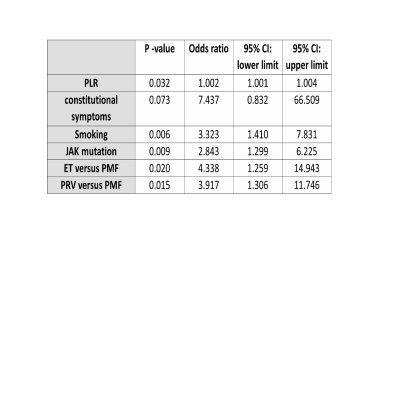
Conclusion
In conclusion, PLR is a strong predictor for thrombosis in patients of MPNs while NLR appears to be higher in the group of patient suffering from thrombosis but not efficiently predict future events. This effect appears independently from other well known risk factors. JAK2 mutation, MPN sub classification and smoking are significantly associated to the burden of thrombotic risk.
Keyword(s): Myeloproliferative disorder, Thrombosis
Abstract: EP1118
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
Major thrombotic events are devastating complications in the Philadelphia negative myeloproliferative diseases. The neutrophil- lymphocyte ratio (NLR) and the platelet- lymphocyte ratio (PLR) were found to be associated with the burden of thrombotic events.
Aims
Our objective is to determine the role of NLR, and PLR ratios detected at the diagnosis of the MPN diseases as an indicator to thrombosis in conjugation with the other risk factors and to illustrate the difference between the patients developed thrombosis at the diagnosis of MPN disease and patients who develop the thrombosis after the diagnosis.
Methods
The current study is a single-center observational prospective cohort (NCT03599700, Clinical Trials.gov) conducted in a university-affiliated hospital (Assiut University Hospital, Assiut, Egypt).
Subjects were enrolled if BCR-ABL negative myeloproliferative neoplasms e.g.: Polycythemia vera, Essential thrombocythemia, and Primary myelofibrosis and the age was more than 18 years.
Clinical and demographic data were collected. Laboratory assessment included complete blood count (CBC). Follow up for thrombotic events were planned for three years from the start of the study. The patients were divided to three groups according to the incidence of thrombosis either no thrombosis or thrombosis at diagnosis of the MPN or thrombosis after the diagnosis of the disease.
Results
Within 15 months of the study, we recruited 204 patients with 142 patients (69.6%) of whom showed no thrombosis and 42 patients (20.6%) of the patients affected by thrombosis at the diagnosis and 20 patients (9.8%) of the patients developed thrombosis during their follow up.
We found that thrombosis at and after diagnosis occurred in 42 patients (27%) at age <65 years while it occurred in 20 patients (40.8%) at age ≥ 65 years group (P=0.05).
PLR showed a significant difference between Patients without thrombosis group and both Patients with thrombosis at diagnosis and after diagnosis groups (P= 0.002).
NLR showed a significant difference between Patients without thrombosis group and the group of Patients with thrombosis at diagnosis and after diagnosis groups (P= 0.03).
Univariate analysis was done for the thrombosis risk factors: sex, BMI, diagnosis subclassification, presence of constitutional symptoms, JAK mutation, PLR, NLR, age ≥65 years and smoking status.
PLR, constitutional symptoms, smoking status, JAK mutation and MPN subclassification were the significant factors and incorporated into multivariate analysis.
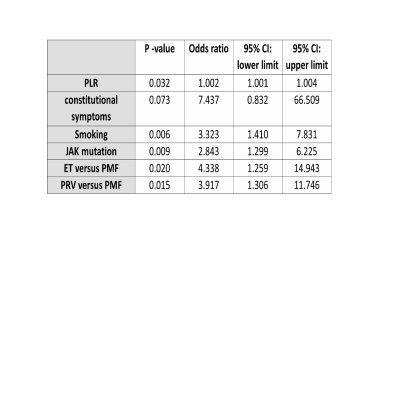
Conclusion
In conclusion, PLR is a strong predictor for thrombosis in patients of MPNs while NLR appears to be higher in the group of patient suffering from thrombosis but not efficiently predict future events. This effect appears independently from other well known risk factors. JAK2 mutation, MPN sub classification and smoking are significantly associated to the burden of thrombotic risk.
Keyword(s): Myeloproliferative disorder, Thrombosis


