
Contributions
Abstract: EP1113
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
In Polycythemia vera (PV) and essential thrombocythemia (ET) morbidity relates to thrombotic events. The JAK2 V617F mutation alters both the cellular and plasma compartments of hemostasis favoring a hypercoagulable state. Compared to a matched control population, PV/ET pts have a significantly increased rate of thrombotic events and this risk remains independent of gender and across all age groups. Conventional cardiovascular risk factors (CRF) add to the risk of acute coronary syndrome (ACS).
Aims
Since ACS can occur either as first clinical manifestation of PV/ET or it may complicate its course, we explored the possibility that differences may exist between these two settings.
Methods
Retrospective cohort study of 1,413 consecutive ACS performed at ASST Niguarda Hospital between Jan 2014 and Dec 2019. Patients were divided into 3 groups: group 1: patients diagnosed with JAK2+ PV/ET during the index hospitalization; group 2: patients with a known diagnosis of JAK2+ PV/ET; group 3: control group = ACS in myeloproliferative neoplasm (MPN) negative pts. Clinical and angiography data and outcome events were compared among the 3 groups.
Results
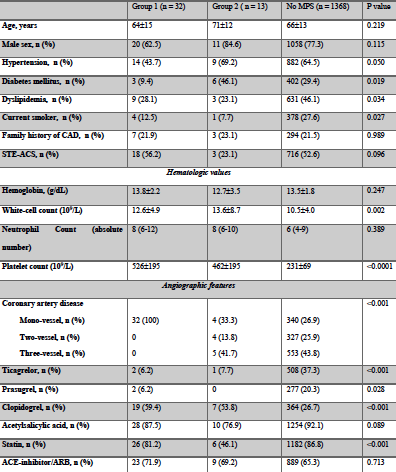
Data are summarized in the Table. Overall, MPN patients differed from MPN negative patients in terms of CRF and extension of coronary artery disease. These differences were even more prominent between MPN group 1 and group 2 patients. Specifically, incidence of CRF was lower and single-vessel disease was more prevalent among group 1 patients. Interestingly, a decreased incidence of long-term adverse cardiovascular events was observed in group 1 MPN patients. At a median follow-up of 18 months, the composite of overall mortality, myocardial infarction, stroke and bleeding events occurred in 2 (6.2%) patients in group 1, in 1 patient (7.7%) in group 2 and 188 patients (13.7%) in MPN-negative ACS patients.
Conclusion
ACS is a known complication of JAK2+ PV/ET. In this setting it displays peculiar angiography features according to time of clinical presentation with newly diagnosed PV/ET patients more often showing single-vessel involvement compared to patients with known PV/ET who have angiography features similar to the control group. CRF were also not significantly represented among these patients. It is tempting to hypothesize that mechanisms other than atherosclerotic plaque rupture may be relevant to ACS development when JAK2+ PV/ET occur. Considering the anatomical sites involved, it may be speculated that endothelial dysfunction associated with elevated shear stress may be the main inciting factor leading to thrombosis. In the setting of shear-induced endothelial dysfunction, the overall pro-coagulant features of circulating cells may give rise to thrombus formation even in the absence of underlying plaques. Recognition by the cardiologists of the peculiar angiography features associated with ACS as initial presentation of PV/ET should prompt hematologic counseling aimed at a tailored treatment strategy. Dual anti-platelet therapy alone may not protect from further thrombotic events and a more comprehensive therapeutic strategy, comprising hydroxycarbamide/phlebotomy, is be advisable in these patients.
Keyword(s): Acute coronary syndrome, Essential Thrombocytemia, Polycythemia vera
Abstract: EP1113
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
In Polycythemia vera (PV) and essential thrombocythemia (ET) morbidity relates to thrombotic events. The JAK2 V617F mutation alters both the cellular and plasma compartments of hemostasis favoring a hypercoagulable state. Compared to a matched control population, PV/ET pts have a significantly increased rate of thrombotic events and this risk remains independent of gender and across all age groups. Conventional cardiovascular risk factors (CRF) add to the risk of acute coronary syndrome (ACS).
Aims
Since ACS can occur either as first clinical manifestation of PV/ET or it may complicate its course, we explored the possibility that differences may exist between these two settings.
Methods
Retrospective cohort study of 1,413 consecutive ACS performed at ASST Niguarda Hospital between Jan 2014 and Dec 2019. Patients were divided into 3 groups: group 1: patients diagnosed with JAK2+ PV/ET during the index hospitalization; group 2: patients with a known diagnosis of JAK2+ PV/ET; group 3: control group = ACS in myeloproliferative neoplasm (MPN) negative pts. Clinical and angiography data and outcome events were compared among the 3 groups.
Results
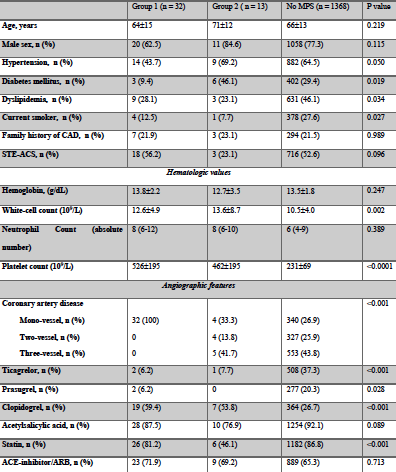
Data are summarized in the Table. Overall, MPN patients differed from MPN negative patients in terms of CRF and extension of coronary artery disease. These differences were even more prominent between MPN group 1 and group 2 patients. Specifically, incidence of CRF was lower and single-vessel disease was more prevalent among group 1 patients. Interestingly, a decreased incidence of long-term adverse cardiovascular events was observed in group 1 MPN patients. At a median follow-up of 18 months, the composite of overall mortality, myocardial infarction, stroke and bleeding events occurred in 2 (6.2%) patients in group 1, in 1 patient (7.7%) in group 2 and 188 patients (13.7%) in MPN-negative ACS patients.
Conclusion
ACS is a known complication of JAK2+ PV/ET. In this setting it displays peculiar angiography features according to time of clinical presentation with newly diagnosed PV/ET patients more often showing single-vessel involvement compared to patients with known PV/ET who have angiography features similar to the control group. CRF were also not significantly represented among these patients. It is tempting to hypothesize that mechanisms other than atherosclerotic plaque rupture may be relevant to ACS development when JAK2+ PV/ET occur. Considering the anatomical sites involved, it may be speculated that endothelial dysfunction associated with elevated shear stress may be the main inciting factor leading to thrombosis. In the setting of shear-induced endothelial dysfunction, the overall pro-coagulant features of circulating cells may give rise to thrombus formation even in the absence of underlying plaques. Recognition by the cardiologists of the peculiar angiography features associated with ACS as initial presentation of PV/ET should prompt hematologic counseling aimed at a tailored treatment strategy. Dual anti-platelet therapy alone may not protect from further thrombotic events and a more comprehensive therapeutic strategy, comprising hydroxycarbamide/phlebotomy, is be advisable in these patients.
Keyword(s): Acute coronary syndrome, Essential Thrombocytemia, Polycythemia vera


