
Contributions
Abstract: EP1099
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
patients with myeloproliferative neoplasms (MPNs) have an intrinsic risk of lymphoproliferative disease (LPD) compared to the general population, ranging from 2.79 to 3.44 folds increased as reported in literature. Less is known about the clinical characteristics of this setting of patients and their outcome in terms of infectious and thrombotic complications.
Aims
to assess the occurrence of infections and thrombosis in patients with concomitant myeloid and lymphoid neoplasms.
Methods
We retrospectively evaluated a single center cohort of 1351 myeloid neoplasms (930 MPN and 421 myelodysplastic syndromes [MDS]) followed up for a median of 9 (0.8-35) years. We evaluated the time from diagnosis to LPD development, LPD type, treatment requirement for both myeloid disorder and LPD, and the occurrence of infections, thrombosis, and overall survival (OS).
Results
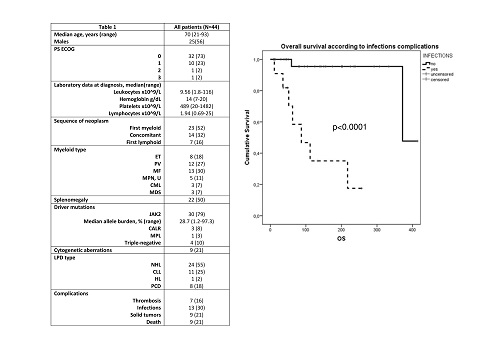
A total of 44 patients developed an LPD after a median of 37 (0-318) months from myeloid disease, in 32% of patients myeloid and lymphoid neoplasms were diagnosed concomitantly. Table 1 shows clinical and laboratory characteristics: patients were mainly males, 61% >65 years, and all but 3 had a diagnosis of MPN. JAK2V617F-mutated patients were 30 (68%), while 25% and 11% were CALR- and MPL-mutated, respectively. Mutated patients showed a longer time to LPD development (mean 120+92 versus 31+17 months in unmutated, p=0.01).
As regards treatment, 29 MPN patients were on anti-platelet therapy, 2 on anticoagulants, 36 (82%) of MPN patients required myeloid specific treatment, the majority with hydroxyurea (71%). Lymphoid disease required treatment in 45.5% of cases, after a median time from diagnosis of 8 months (0-115). A thrombotic event was reported in seven patients (4 ET and 3 MF), and, unexpectedly, JAK2 resulted unmutated in more than half of the cases (57.1%). Thirteen patients (30%) experienced a grade >3 infectious episode (9 pneumonias, 3 urinary tract infection, and 1 sepsis), all due to bacterial agents, occurring mainly in elderly subjects (12/13, p=0.006).
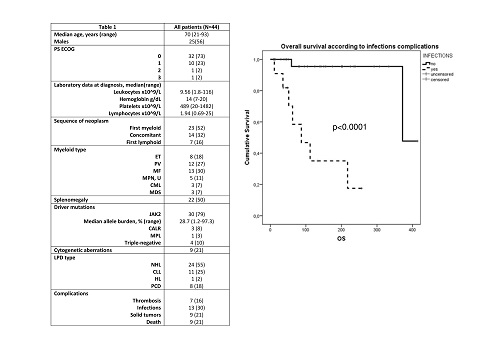
Nine patients (20%) died due to solid tumor (4), leukemic progression (2), infectious complications (2), and brain bleeding (1). Deaths were more frequent among elderly patients (89%), ECOG >1 (42% versus 13%, p=0.02), and triple-negative status (50% versus 12.5%, p=0.02); deaths were also associated with a significantly shorter time to LPD development (37+8 versus 115+94 months, p=0.002) and with lymphoid treatment requirement (35% versus 9%, p=0.04). In addition, fatalities were more frequent in patients with infections (58% versus 6%, p=0.001). By Kaplan Meyer method, a longer OS was observed in younger patients (p=0.001), with better performance status (p=0.02) and with the presence of driver mutations (p=0.003). Contrarily, a worse survival was significantly associated with the occurrence of infections (p<0.0001). Multivariate analysis by Cox regression model showed that the occurrence of infections was the only independent predictor of worse survival within the cohort (HR 3.18, 95%CI 2.9-19, p=0.003).
Conclusion
The co-occurence of LPD and myeloid neoplasms was associated with a high rate of infectious complications (30%) being the latter the only independent predictor of shorter OS. Interestingly, our data support the adverse prognostic impact of triple-negative molecular status also in this specific setting.
Keyword(s): Infection, Lymphoproliferative disorder, Myeloproliferative disorder, Thrombosis
Abstract: EP1099
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
patients with myeloproliferative neoplasms (MPNs) have an intrinsic risk of lymphoproliferative disease (LPD) compared to the general population, ranging from 2.79 to 3.44 folds increased as reported in literature. Less is known about the clinical characteristics of this setting of patients and their outcome in terms of infectious and thrombotic complications.
Aims
to assess the occurrence of infections and thrombosis in patients with concomitant myeloid and lymphoid neoplasms.
Methods
We retrospectively evaluated a single center cohort of 1351 myeloid neoplasms (930 MPN and 421 myelodysplastic syndromes [MDS]) followed up for a median of 9 (0.8-35) years. We evaluated the time from diagnosis to LPD development, LPD type, treatment requirement for both myeloid disorder and LPD, and the occurrence of infections, thrombosis, and overall survival (OS).
Results
A total of 44 patients developed an LPD after a median of 37 (0-318) months from myeloid disease, in 32% of patients myeloid and lymphoid neoplasms were diagnosed concomitantly. Table 1 shows clinical and laboratory characteristics: patients were mainly males, 61% >65 years, and all but 3 had a diagnosis of MPN. JAK2V617F-mutated patients were 30 (68%), while 25% and 11% were CALR- and MPL-mutated, respectively. Mutated patients showed a longer time to LPD development (mean 120+92 versus 31+17 months in unmutated, p=0.01).
As regards treatment, 29 MPN patients were on anti-platelet therapy, 2 on anticoagulants, 36 (82%) of MPN patients required myeloid specific treatment, the majority with hydroxyurea (71%). Lymphoid disease required treatment in 45.5% of cases, after a median time from diagnosis of 8 months (0-115). A thrombotic event was reported in seven patients (4 ET and 3 MF), and, unexpectedly, JAK2 resulted unmutated in more than half of the cases (57.1%). Thirteen patients (30%) experienced a grade >3 infectious episode (9 pneumonias, 3 urinary tract infection, and 1 sepsis), all due to bacterial agents, occurring mainly in elderly subjects (12/13, p=0.006).
Nine patients (20%) died due to solid tumor (4), leukemic progression (2), infectious complications (2), and brain bleeding (1). Deaths were more frequent among elderly patients (89%), ECOG >1 (42% versus 13%, p=0.02), and triple-negative status (50% versus 12.5%, p=0.02); deaths were also associated with a significantly shorter time to LPD development (37+8 versus 115+94 months, p=0.002) and with lymphoid treatment requirement (35% versus 9%, p=0.04). In addition, fatalities were more frequent in patients with infections (58% versus 6%, p=0.001). By Kaplan Meyer method, a longer OS was observed in younger patients (p=0.001), with better performance status (p=0.02) and with the presence of driver mutations (p=0.003). Contrarily, a worse survival was significantly associated with the occurrence of infections (p<0.0001). Multivariate analysis by Cox regression model showed that the occurrence of infections was the only independent predictor of worse survival within the cohort (HR 3.18, 95%CI 2.9-19, p=0.003).
Conclusion
The co-occurence of LPD and myeloid neoplasms was associated with a high rate of infectious complications (30%) being the latter the only independent predictor of shorter OS. Interestingly, our data support the adverse prognostic impact of triple-negative molecular status also in this specific setting.
Keyword(s): Infection, Lymphoproliferative disorder, Myeloproliferative disorder, Thrombosis


