Contributions
Abstract: EP1096
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
Patients with myelofibrosis (MF) have decreased overall survival with a median of 5 years. Leading causes of death are believed to be directly or indirectly related to MF progression or complications, including transformation to acute leukemia (AML) and infections.
Aims
We aimed to compare survival, mortality rate and causes of death of MF patients referred to our institution before (≤) and after the years of 2010.
Methods
This retrospective study included patients with MF diagnosed within one year prior to their presentation to our institution (between January 1990 and February 2020, 4% presented < year 2000). Patients with unknown cause of death or loss to follow-up were excluded (final cohort, n = 995). Causes of death were divided into groups: i) MF progression; ii) AML (≥ 20% blasts); iii) sudden multi-organ failure or vascular event (possibly related to MF, Vasc/MOF); iii) infections (MF had to be controlled or in remission); iv) other (unrelated medical conditions). We calculated crude mortality rate per 1000 person - years of observation (comparison by Poisson’s regression) and overall survival (by Kaplan Meier method with log rank test). To account for variations in age groups (< 49; 50-59; 60-69; and 70+ years), we assessed age-adjusted mortality rates per 1000 person-years standardized for the entire cohort.
Results
The study included 378 and 617 patients ≤ and > 2010, respectively, 59% of which were males. Sixty-five percent of patients were ≥60 years. Distribution of age groups between periods was comparable, except for higher proportion of 70+ year old patients > 2010, counterbalanced by lower proportion of < 60 years.
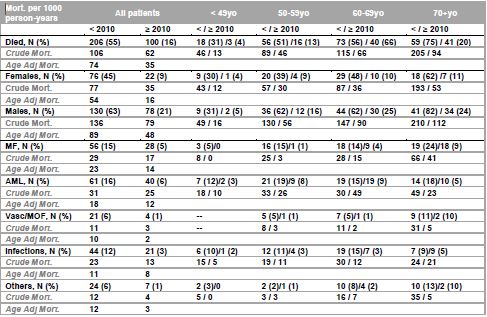
Over the observation time of 1942 and 1608 person-years for ≤ and > 2010, 206 (55%) and 100 (16%) of patients died, respectively (p < 0.001, RR 0.54, CI 0.48-0.63). Crude, age-adjusted and cause-specific mortality per 1000 person-years in both periods is outlined in Table.
Overall mortality, both crude and age-adjusted, was significantly higher ≤ 2010 irrespectively of gender and age. As expected, crude mortality steadily increased with age in both periods. For each of the respective age groups, more patients died ≤ 2010 than > 2010. In both periods, males had higher mortality than females; but it has decreased > 2010 for both genders. Whilst comparable death rate was observed between < 49 years males and females, it was significantly higher in males for all other ages regardless of periods.
Leading cause of mortality for all combined ages was AML, followed by MF, infections, Vasc/MOF and other causes. However, when MF related and possibly related causes of death (Vasc/MOF, or /i+iii/) were combined, this group was leading cause of mortality ≤ 2010, and was comparable to AML > 2010. Cause specific crude mortality has decreased > 2010 for all subcategories, except for AML, which remained unchanged between periods. MF and AML related cause of deaths were increasing with age irrespectively of periods (Table).
Conclusion
In our study, we provide specific details on overall and cause specific mortality for patients with MF and show declining rates in the last decade (> 2010). However, the leading cause of death still remain MF and AML, implying ongoing need for clinical research and novel therapies.
Keyword(s):
Abstract: EP1096
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
Patients with myelofibrosis (MF) have decreased overall survival with a median of 5 years. Leading causes of death are believed to be directly or indirectly related to MF progression or complications, including transformation to acute leukemia (AML) and infections.
Aims
We aimed to compare survival, mortality rate and causes of death of MF patients referred to our institution before (≤) and after the years of 2010.
Methods
This retrospective study included patients with MF diagnosed within one year prior to their presentation to our institution (between January 1990 and February 2020, 4% presented < year 2000). Patients with unknown cause of death or loss to follow-up were excluded (final cohort, n = 995). Causes of death were divided into groups: i) MF progression; ii) AML (≥ 20% blasts); iii) sudden multi-organ failure or vascular event (possibly related to MF, Vasc/MOF); iii) infections (MF had to be controlled or in remission); iv) other (unrelated medical conditions). We calculated crude mortality rate per 1000 person - years of observation (comparison by Poisson’s regression) and overall survival (by Kaplan Meier method with log rank test). To account for variations in age groups (< 49; 50-59; 60-69; and 70+ years), we assessed age-adjusted mortality rates per 1000 person-years standardized for the entire cohort.
Results
The study included 378 and 617 patients ≤ and > 2010, respectively, 59% of which were males. Sixty-five percent of patients were ≥60 years. Distribution of age groups between periods was comparable, except for higher proportion of 70+ year old patients > 2010, counterbalanced by lower proportion of < 60 years.
Over the observation time of 1942 and 1608 person-years for ≤ and > 2010, 206 (55%) and 100 (16%) of patients died, respectively (p < 0.001, RR 0.54, CI 0.48-0.63). Crude, age-adjusted and cause-specific mortality per 1000 person-years in both periods is outlined in Table.
Overall mortality, both crude and age-adjusted, was significantly higher ≤ 2010 irrespectively of gender and age. As expected, crude mortality steadily increased with age in both periods. For each of the respective age groups, more patients died ≤ 2010 than > 2010. In both periods, males had higher mortality than females; but it has decreased > 2010 for both genders. Whilst comparable death rate was observed between < 49 years males and females, it was significantly higher in males for all other ages regardless of periods.
Leading cause of mortality for all combined ages was AML, followed by MF, infections, Vasc/MOF and other causes. However, when MF related and possibly related causes of death (Vasc/MOF, or /i+iii/) were combined, this group was leading cause of mortality ≤ 2010, and was comparable to AML > 2010. Cause specific crude mortality has decreased > 2010 for all subcategories, except for AML, which remained unchanged between periods. MF and AML related cause of deaths were increasing with age irrespectively of periods (Table).
Conclusion
In our study, we provide specific details on overall and cause specific mortality for patients with MF and show declining rates in the last decade (> 2010). However, the leading cause of death still remain MF and AML, implying ongoing need for clinical research and novel therapies.
Keyword(s):