
Contributions
Abstract: EP1091
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
Vascular complications such as thrombosis and hemorrhage are major causes of morbimortality in patients with essential thrombocythemia (ET). The 2016 revised IPSET-thrombosis (R-IPSET-thrombosis) score stratifies patients into very-low (VLR), low (LR), intermediate (IR) and high (HR) risk groups according to thrombosis history, age≥60 years and JAK2mut. Such stratification is important as lower risk patients receive less intensive treatment.
Aims
Confirm the prognostic impact of the R-IPSET-thrombosis risk score and other risk factors for thrombosis and major bleeding in a large cohort of adult patients with ET.
Methods
Medical records were retrospectively reviewed for data on thrombotic events, major hemorrhages; and anti-aggregation, anticoagulation, and cytoreductive treatment for 1381 adult ET from 1 French, 1 Italian, 3 Spanish and 5 Polish hospitals. Patients were treated according to local protocols. Statistical analyses were performed using R Core Team 2020 software v4.0.2.
Results
Patient median age was 62 years (54.4% ≥60 years). In terms of driver mutation, 898 were mutated in JAK2 (65.0%), 264 (19.1%) in CALR, and 24 (1.7%) in MPL; 176 (12.7%) were triple negative (19 patients were negative for JAK2 and CALR but MPL was not determined).
Data on thrombosis and major bleeding was available for 1378 and 1380 patients, respectively. With an average follow-up period of 87.7 months, a total of 91 hemorrhagic events (6.6%) were reported. Thrombotic events occurred in 260 patients (18.8%) before or at diagnosis (dx), and in 173 patients (12.6%) after dx. There were 88 deaths (6.4% of the study population).
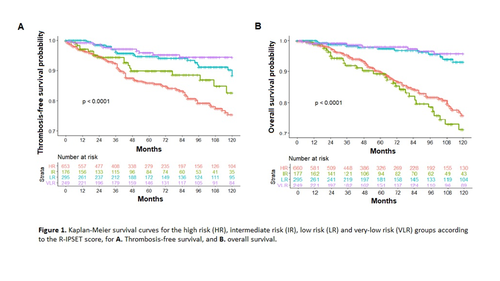
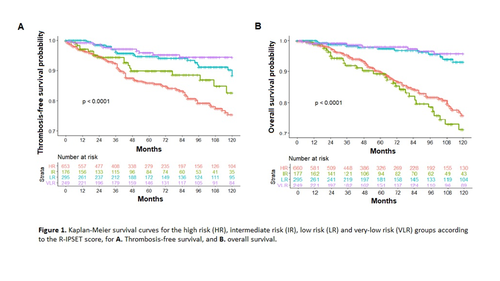
Following distribution into risk groups according to the R-IPSET-thrombosis score, thrombosis-free survival (TFS) at 10 years for the VLR, LR, IR and HR groups was 99%, 88%, 83% and 75%, respectively (p<0.0001). Overall survival (OS) according to thrombosis risk group was 96%, 93%, 76% and 71%, respectively (p<0.0001) (Figure 1). Comparing the LR and VLR groups, the difference in TFS was significant (Fisher Exact test, p<0.001) but OS was not (HR 1.43, p=0.451).
Logistic regression univariate analysis confirmed the R-IPSET-thrombosis variables of age at dx, cardiovascular risk factors, thrombosis history, and JAK2mut as thrombotic risk factors (HR 2.5, 1.9, 2.3, and 1.6, respectively). CALRmut was a protective factor (HR 0.43, p=0.0021). In multivariate analysis, only age, previous thrombosis and CALRmut retained statistical significance. For thrombotic event prior to dx or at dx, JAK2mut was a risk factor (Fisher exact, OR 2.8, p<0.001) while CALRmut was a protective factor (OR 0.32, p<0.001); MPLmut was not a significant risk factor.
For major bleeding, leukocyte count was a significant risk factor while hemoglobin count was a significant protective factor in multivariate analysis.
Anti-aggregation after dx had a protective effect on thrombosis (HR 0.31, p=0.005) in multivariate analysis but was not protective for major bleeding (χ2, p=0.708). Thrombosis at 10 years was not a significant risk factor (HR 1.3, p=0.35) for OS while severe bleeding was (HR 2.3, p=0.0011). Among the 249 patients in the VLR group, 12 had severe bleeding (4.8%), of which 9 received anti-aggregation (75%).
Conclusion
TFS was significantly different between the risk groups; specifically, the VLR group had a higher TFS than the LR group. Therefore, our results validate the R-IPSET score. Anti-aggregation after dx was protective for thrombosis but not for major bleeding. Major bleeding at 10 years was associated with mortality but thrombosis was not.
Keyword(s): Hemorrhage, Prognostic groups, Thromboembolic events
Abstract: EP1091
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
Vascular complications such as thrombosis and hemorrhage are major causes of morbimortality in patients with essential thrombocythemia (ET). The 2016 revised IPSET-thrombosis (R-IPSET-thrombosis) score stratifies patients into very-low (VLR), low (LR), intermediate (IR) and high (HR) risk groups according to thrombosis history, age≥60 years and JAK2mut. Such stratification is important as lower risk patients receive less intensive treatment.
Aims
Confirm the prognostic impact of the R-IPSET-thrombosis risk score and other risk factors for thrombosis and major bleeding in a large cohort of adult patients with ET.
Methods
Medical records were retrospectively reviewed for data on thrombotic events, major hemorrhages; and anti-aggregation, anticoagulation, and cytoreductive treatment for 1381 adult ET from 1 French, 1 Italian, 3 Spanish and 5 Polish hospitals. Patients were treated according to local protocols. Statistical analyses were performed using R Core Team 2020 software v4.0.2.
Results
Patient median age was 62 years (54.4% ≥60 years). In terms of driver mutation, 898 were mutated in JAK2 (65.0%), 264 (19.1%) in CALR, and 24 (1.7%) in MPL; 176 (12.7%) were triple negative (19 patients were negative for JAK2 and CALR but MPL was not determined).
Data on thrombosis and major bleeding was available for 1378 and 1380 patients, respectively. With an average follow-up period of 87.7 months, a total of 91 hemorrhagic events (6.6%) were reported. Thrombotic events occurred in 260 patients (18.8%) before or at diagnosis (dx), and in 173 patients (12.6%) after dx. There were 88 deaths (6.4% of the study population).
Following distribution into risk groups according to the R-IPSET-thrombosis score, thrombosis-free survival (TFS) at 10 years for the VLR, LR, IR and HR groups was 99%, 88%, 83% and 75%, respectively (p<0.0001). Overall survival (OS) according to thrombosis risk group was 96%, 93%, 76% and 71%, respectively (p<0.0001) (Figure 1). Comparing the LR and VLR groups, the difference in TFS was significant (Fisher Exact test, p<0.001) but OS was not (HR 1.43, p=0.451).
Logistic regression univariate analysis confirmed the R-IPSET-thrombosis variables of age at dx, cardiovascular risk factors, thrombosis history, and JAK2mut as thrombotic risk factors (HR 2.5, 1.9, 2.3, and 1.6, respectively). CALRmut was a protective factor (HR 0.43, p=0.0021). In multivariate analysis, only age, previous thrombosis and CALRmut retained statistical significance. For thrombotic event prior to dx or at dx, JAK2mut was a risk factor (Fisher exact, OR 2.8, p<0.001) while CALRmut was a protective factor (OR 0.32, p<0.001); MPLmut was not a significant risk factor.
For major bleeding, leukocyte count was a significant risk factor while hemoglobin count was a significant protective factor in multivariate analysis.
Anti-aggregation after dx had a protective effect on thrombosis (HR 0.31, p=0.005) in multivariate analysis but was not protective for major bleeding (χ2, p=0.708). Thrombosis at 10 years was not a significant risk factor (HR 1.3, p=0.35) for OS while severe bleeding was (HR 2.3, p=0.0011). Among the 249 patients in the VLR group, 12 had severe bleeding (4.8%), of which 9 received anti-aggregation (75%).
Conclusion
TFS was significantly different between the risk groups; specifically, the VLR group had a higher TFS than the LR group. Therefore, our results validate the R-IPSET score. Anti-aggregation after dx was protective for thrombosis but not for major bleeding. Major bleeding at 10 years was associated with mortality but thrombosis was not.
Keyword(s): Hemorrhage, Prognostic groups, Thromboembolic events


