
Contributions
Abstract: EP1090
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
Patients with myeloproliferative neoplasms (MPN) are at increased risk of venous and arterial thromboembolic events (TEEs). Although MPN-specific treatment is generally delivered by specialist haematology centres in the United Kingdom (UK), cardiovascular risk is managed in the primary care setting. In the UK, primary care is provided by the government-funded National Health Service, and patient data is collected by the Clinical Practice Research Datalink (CPRD).
Aims
In this retrospective cohort study, we interrogated the CPRD, a centralized national dataset comprising clinical and prescription records for patients in primary care across the entire UK, for descriptive data on the cardiovascular health and thrombotic risk of all patients with MPN.
Methods
During the study period (1 Jan 2012–21 Aug 2019), adults were indexed at the date of first recorded diagnosis for polycythemia vera (PV), essential thrombocythemia (ET) and primary myelofibrosis (MF), with a ≥6-month pre-index lookback and ≥24-month post-index follow-up. The study objectives were to determine the MPN epidemiological landscape, extent of co-morbidities (using the Charlson score), thrombotic/cardiovascular risk profiles (before diagnosis) and occurrence of TEEs/cardiovascular events (CVEs) (after diagnosis). MPN diagnoses and co-morbidities were determined using medical and ICD-10 codes; medications were identified using product codes.
Results
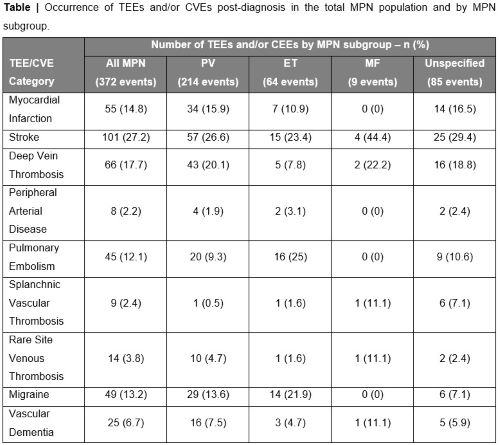
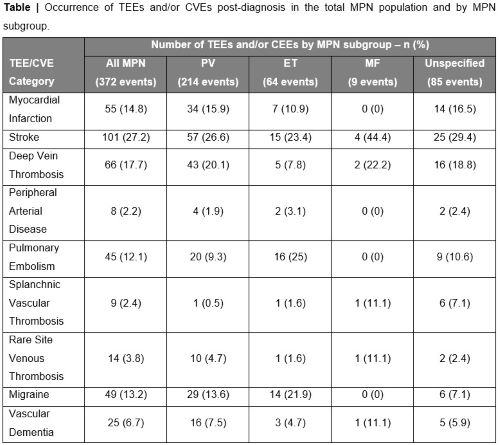
Overall, 2,477 patients with MPN (PV, n=1,315; ET, n=336; MF, n=146; unspecified MPN, n=680) of the 19,474,733 patients in the CPRD were identified with a median age at diagnosis of 68 years (range 7 months–101 years); 56% were male. Among all MPN patients, 96.2% had a low Charlson co-morbidity score of 0–5. The prevalence of MPN was 12.72 per 100,000; PV was the most prevalent MPN subtype (6.75 per 100,000), followed by ET (1.73 per 100,000) and MF (0.75 per 100,000). In the total MPN population, the most prevalent pre-diagnosis risk factors were smoking (59.8%) and ischaemic heart disease (27.7%); few patients had hypertension (14.6%), diabetes (13.1%), dyslipidaemia (12.8%) or obesity (8.8%). For risk management, most hypertensive (88.9%), dyslipidemic (82.4%) and diabetic (77.9%) patients were prescribed appropriate medications for management of their blood pressure, dyslipidemia, and diabetes, respectively. Among the patient cohort, 372 TEEs/CVEs occurred after diagnosis (PV, 214 events; ET, 64 events; MF, 9 events; unspecified MPN, 85 events), the most common being stroke (27.2%), deep vein thrombosis (17.7%) and myocardial infarction (MI; 14.8%) (Table). Notably, the occurrence of MI was greater for patients with PV (15.9%) than for those with ET (10.9%) or MF (0%).
Conclusion
This study is the first of its kind to describe the cardiovascular health and thrombotic risk profiles of UK patients with MPN in primary care within the CPRD. The prevalence of PV and MF in this study was largely consistent with most known epidemiological reports, but the prevalence of ET was lower. However, MPN subtype was not specified in the CPRD for a sizeable proportion (680 of 2,477 patients). Importantly, in the UK MPN population, the majority were smokers and a considerable proportion of patients (11.1–22.1%) were not prescribed appropriate medications for management of co-morbidities associated with thrombotic risk (hypertension, dyslipidemia or diabetes), highlighting a potential unmet need for improved cardiovascular risk management and coordination between primary and secondary care.
Keyword(s): Epidemiology, Myeloproliferative disorder, Thromboembolic events
Abstract: EP1090
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
Patients with myeloproliferative neoplasms (MPN) are at increased risk of venous and arterial thromboembolic events (TEEs). Although MPN-specific treatment is generally delivered by specialist haematology centres in the United Kingdom (UK), cardiovascular risk is managed in the primary care setting. In the UK, primary care is provided by the government-funded National Health Service, and patient data is collected by the Clinical Practice Research Datalink (CPRD).
Aims
In this retrospective cohort study, we interrogated the CPRD, a centralized national dataset comprising clinical and prescription records for patients in primary care across the entire UK, for descriptive data on the cardiovascular health and thrombotic risk of all patients with MPN.
Methods
During the study period (1 Jan 2012–21 Aug 2019), adults were indexed at the date of first recorded diagnosis for polycythemia vera (PV), essential thrombocythemia (ET) and primary myelofibrosis (MF), with a ≥6-month pre-index lookback and ≥24-month post-index follow-up. The study objectives were to determine the MPN epidemiological landscape, extent of co-morbidities (using the Charlson score), thrombotic/cardiovascular risk profiles (before diagnosis) and occurrence of TEEs/cardiovascular events (CVEs) (after diagnosis). MPN diagnoses and co-morbidities were determined using medical and ICD-10 codes; medications were identified using product codes.
Results
Overall, 2,477 patients with MPN (PV, n=1,315; ET, n=336; MF, n=146; unspecified MPN, n=680) of the 19,474,733 patients in the CPRD were identified with a median age at diagnosis of 68 years (range 7 months–101 years); 56% were male. Among all MPN patients, 96.2% had a low Charlson co-morbidity score of 0–5. The prevalence of MPN was 12.72 per 100,000; PV was the most prevalent MPN subtype (6.75 per 100,000), followed by ET (1.73 per 100,000) and MF (0.75 per 100,000). In the total MPN population, the most prevalent pre-diagnosis risk factors were smoking (59.8%) and ischaemic heart disease (27.7%); few patients had hypertension (14.6%), diabetes (13.1%), dyslipidaemia (12.8%) or obesity (8.8%). For risk management, most hypertensive (88.9%), dyslipidemic (82.4%) and diabetic (77.9%) patients were prescribed appropriate medications for management of their blood pressure, dyslipidemia, and diabetes, respectively. Among the patient cohort, 372 TEEs/CVEs occurred after diagnosis (PV, 214 events; ET, 64 events; MF, 9 events; unspecified MPN, 85 events), the most common being stroke (27.2%), deep vein thrombosis (17.7%) and myocardial infarction (MI; 14.8%) (Table). Notably, the occurrence of MI was greater for patients with PV (15.9%) than for those with ET (10.9%) or MF (0%).
Conclusion
This study is the first of its kind to describe the cardiovascular health and thrombotic risk profiles of UK patients with MPN in primary care within the CPRD. The prevalence of PV and MF in this study was largely consistent with most known epidemiological reports, but the prevalence of ET was lower. However, MPN subtype was not specified in the CPRD for a sizeable proportion (680 of 2,477 patients). Importantly, in the UK MPN population, the majority were smokers and a considerable proportion of patients (11.1–22.1%) were not prescribed appropriate medications for management of co-morbidities associated with thrombotic risk (hypertension, dyslipidemia or diabetes), highlighting a potential unmet need for improved cardiovascular risk management and coordination between primary and secondary care.
Keyword(s): Epidemiology, Myeloproliferative disorder, Thromboembolic events


