
Contributions
Abstract: EP1088
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
A significant proportion, 10-15%, of patients with myeloproliferative neoplasms (MPNs) are of fertile age at diagnosis. Pregnancy in MPN patients is associated with increased risks of numerous complications, including bleeding, thrombosis, and fetal loss. Population-based studies of pregnancy outcomes in MPN patients are rare, and even less is known about risks for the child.
Aims
The aim of this study is to assess adverse pregnancy outcomes in patients with MPN in a population-based setting.
Methods
Patients with MPN were identified in the Swedish Cancer Register and Patient Registers, from 1953 to 2019. All pregnancies in these patients between 1973 and 2019 were identified from the Medical Birth Register, which captures all pregnancies in Sweden starting from gestational week 22 (before 2008 from week 28), thus only viable pregnancies at that gestational week are included in this study. Women with an MPN diagnosis prior to delivery or during the postpartum period (2 months) were included. From the general population, one pregnant control per pregnant MPN patient was randomly selected, matched by maternal age, year of delivery, maternal parity, and whether it was a singleton or duplex pregnancy. Main outcomes were stillbirth, birthweight, small-for-gestational-age, and preterm birth. The two-sided Fisher exact test was used to assess associations, with p-values <0.05 considered statistically significant. In the test comparison, only the first pregnancy after MPN was included.
Results
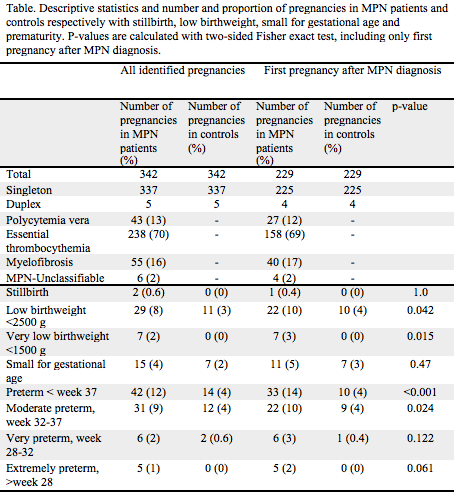
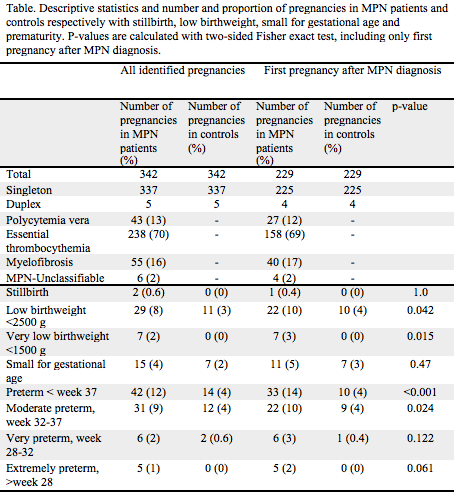
We identified 342 pregnancies in 229 women with MPN, and equally many in controls, 337 of these were singleton pregnancies and 5 duplex pregnancies, table. Among the 342 pregnancies in MPN patients, 43 were in patients with polycythemia vera, 238 in patients with essential thrombocythemia, 55 in patients with primary myelofibrosis and 6 in patients with MPN-unclassifiable. The mean maternal age at delivery among MPN patients and controls was 31.9 years, range 20-45. Mean birthweight was 3,378 g in children to MPN patients and 3,573 g in controls.
When restricting to first pregnancy after MPN, there were 229 pregnancies. There was a significantly increased proportion of preterm birth (<37 weeks) in MPN patients (n=33, 14%) compared to controls (n=10, 4%). Furthermore, 11 deliveries were very (week 28-32) or extremely (<28 weeks) preterm in MPN patients, compared to 1 in the control group. The proportion of neonates with low birthweight was also significantly higher in MPN patients (n=22, 10%) versus in controls (n=10, 4%). No significant differences were observed in proportion of small-for-gestational-age or stillbirth, although very few events. There was one neonatal death in the MPN group and one in the control group, both on day 2.
Conclusion
This large register- and population-based study demonstrated a significantly increased risk of preterm birth in patients with MPN. The higher proportion of low birthweight in children of MPN patients was mainly but not solely driven by the higher proportion of preterm birth. Our novel findings indicate the need for further clarification of the underlying pathophysiology as well as identification of adequate preventative measures. Preterm birth may affect neonatal morbidity and mortality, and have consequences on future health and capabilities, therefore optimizing care in MPN pregnancies to prevent maternal and neonatal complications is of great importance.
Keyword(s): Essential Thrombocytemia, Myeloproliferative disorder, Polycythemia vera, Pregnancy
Abstract: EP1088
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
A significant proportion, 10-15%, of patients with myeloproliferative neoplasms (MPNs) are of fertile age at diagnosis. Pregnancy in MPN patients is associated with increased risks of numerous complications, including bleeding, thrombosis, and fetal loss. Population-based studies of pregnancy outcomes in MPN patients are rare, and even less is known about risks for the child.
Aims
The aim of this study is to assess adverse pregnancy outcomes in patients with MPN in a population-based setting.
Methods
Patients with MPN were identified in the Swedish Cancer Register and Patient Registers, from 1953 to 2019. All pregnancies in these patients between 1973 and 2019 were identified from the Medical Birth Register, which captures all pregnancies in Sweden starting from gestational week 22 (before 2008 from week 28), thus only viable pregnancies at that gestational week are included in this study. Women with an MPN diagnosis prior to delivery or during the postpartum period (2 months) were included. From the general population, one pregnant control per pregnant MPN patient was randomly selected, matched by maternal age, year of delivery, maternal parity, and whether it was a singleton or duplex pregnancy. Main outcomes were stillbirth, birthweight, small-for-gestational-age, and preterm birth. The two-sided Fisher exact test was used to assess associations, with p-values <0.05 considered statistically significant. In the test comparison, only the first pregnancy after MPN was included.
Results
We identified 342 pregnancies in 229 women with MPN, and equally many in controls, 337 of these were singleton pregnancies and 5 duplex pregnancies, table. Among the 342 pregnancies in MPN patients, 43 were in patients with polycythemia vera, 238 in patients with essential thrombocythemia, 55 in patients with primary myelofibrosis and 6 in patients with MPN-unclassifiable. The mean maternal age at delivery among MPN patients and controls was 31.9 years, range 20-45. Mean birthweight was 3,378 g in children to MPN patients and 3,573 g in controls.
When restricting to first pregnancy after MPN, there were 229 pregnancies. There was a significantly increased proportion of preterm birth (<37 weeks) in MPN patients (n=33, 14%) compared to controls (n=10, 4%). Furthermore, 11 deliveries were very (week 28-32) or extremely (<28 weeks) preterm in MPN patients, compared to 1 in the control group. The proportion of neonates with low birthweight was also significantly higher in MPN patients (n=22, 10%) versus in controls (n=10, 4%). No significant differences were observed in proportion of small-for-gestational-age or stillbirth, although very few events. There was one neonatal death in the MPN group and one in the control group, both on day 2.
Conclusion
This large register- and population-based study demonstrated a significantly increased risk of preterm birth in patients with MPN. The higher proportion of low birthweight in children of MPN patients was mainly but not solely driven by the higher proportion of preterm birth. Our novel findings indicate the need for further clarification of the underlying pathophysiology as well as identification of adequate preventative measures. Preterm birth may affect neonatal morbidity and mortality, and have consequences on future health and capabilities, therefore optimizing care in MPN pregnancies to prevent maternal and neonatal complications is of great importance.
Keyword(s): Essential Thrombocytemia, Myeloproliferative disorder, Polycythemia vera, Pregnancy


