
Contributions
Abstract: EP1081
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
Momelotinib (MMB) is a potent JAK1, JAK2 and ACVR1 inhibitor with clinical activity against the hallmark features of myelofibrosis (MF), namely anemia, constitutional symptoms and splenomegaly, across the continuum of JAKi naïve or previously JAKi treated intermediate/high risk MF patients as demonstrated in the previously conducted Phase 3 SIMPLIFY-1 & -2 clinical trials (S1, S2). S1 was conducted in JAKi-naïve patients with MF (n=432) double-blind randomized 1:1 to MMB or ruxolitinib (RUX).
MMB demonstrated a statistically non-inferior splenic response rate (SRR) to RUX at the W24 landmark analysis in S1 but did not meet significance for total symptom score (TSS) response. Low SRR and TSS response was observed for RUX in patients with low platelets, while MMB elicited consistent SRR and TSS response across the platelet subsets, comparable to the response in the ITT. Transfusion independence (TI) at W24 was higher for MMB vs RUX patients across all PLT strata.
Aims
Progressive anemia is a common occurrence in MF with nearly all MF patients requiring transfusions as their disease advances. Given the prognostic importance of Hgb and transfusion status in MF patients including evidence that achieving or maintaining transfusion independence by Week 24 with momelotinib is associated with improved OS in S1 and S2, we expanded the previously reported retrospective platelet subset analysis.
Methods
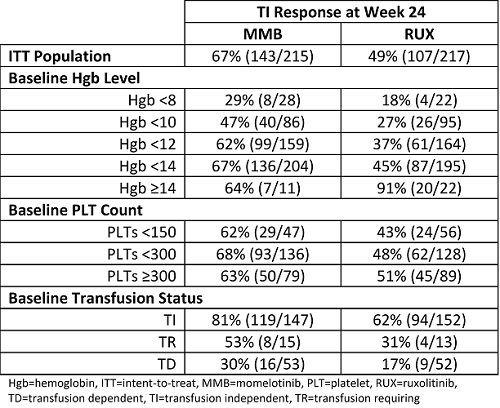
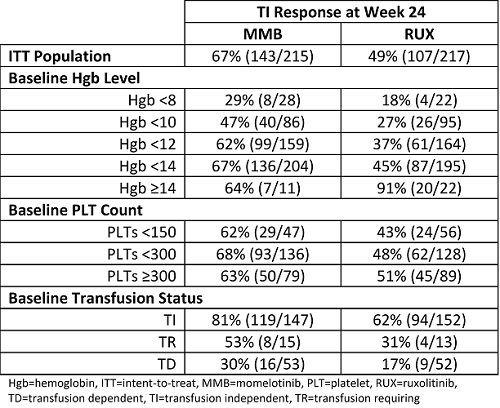
Week 24 TI response rates for MMB and RUX randomized patients in S1 by baseline Hgb and PLT levels and transfusion status were explored.
Results
The data presented here suggest that the prognostically-important W24 TI rate was substantively higher in anemic patients receiving MMB versus RUX, irrespective of the degree of anemia. MMB is also more effective relative to RUX in achieving or maintaining TI in JAKi naïve patients irrespective of baseline PLT count or baseline transfusion status.
Conclusion
Together with data suggesting that TI response at W24 with momelotinib is associated with a survival advantage, these data further support the potential TI benefits of inhibiting ACVR1 in addition to JAK1 and JAK2 with MMB in MF patients.
Keyword(s): Anemia, Janus Kinase inhibitor, Myelofibrosis, Thrombocytopenia
Abstract: EP1081
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
Momelotinib (MMB) is a potent JAK1, JAK2 and ACVR1 inhibitor with clinical activity against the hallmark features of myelofibrosis (MF), namely anemia, constitutional symptoms and splenomegaly, across the continuum of JAKi naïve or previously JAKi treated intermediate/high risk MF patients as demonstrated in the previously conducted Phase 3 SIMPLIFY-1 & -2 clinical trials (S1, S2). S1 was conducted in JAKi-naïve patients with MF (n=432) double-blind randomized 1:1 to MMB or ruxolitinib (RUX).
MMB demonstrated a statistically non-inferior splenic response rate (SRR) to RUX at the W24 landmark analysis in S1 but did not meet significance for total symptom score (TSS) response. Low SRR and TSS response was observed for RUX in patients with low platelets, while MMB elicited consistent SRR and TSS response across the platelet subsets, comparable to the response in the ITT. Transfusion independence (TI) at W24 was higher for MMB vs RUX patients across all PLT strata.
Aims
Progressive anemia is a common occurrence in MF with nearly all MF patients requiring transfusions as their disease advances. Given the prognostic importance of Hgb and transfusion status in MF patients including evidence that achieving or maintaining transfusion independence by Week 24 with momelotinib is associated with improved OS in S1 and S2, we expanded the previously reported retrospective platelet subset analysis.
Methods
Week 24 TI response rates for MMB and RUX randomized patients in S1 by baseline Hgb and PLT levels and transfusion status were explored.
Results
The data presented here suggest that the prognostically-important W24 TI rate was substantively higher in anemic patients receiving MMB versus RUX, irrespective of the degree of anemia. MMB is also more effective relative to RUX in achieving or maintaining TI in JAKi naïve patients irrespective of baseline PLT count or baseline transfusion status.
Conclusion
Together with data suggesting that TI response at W24 with momelotinib is associated with a survival advantage, these data further support the potential TI benefits of inhibiting ACVR1 in addition to JAK1 and JAK2 with MMB in MF patients.
Keyword(s): Anemia, Janus Kinase inhibitor, Myelofibrosis, Thrombocytopenia


