
Contributions
Abstract: EP1072
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Biology & Translational Research
Background
Myeloproliferative neoplasms (MPNs) like Essential Thrombocythemia (ET) presents with higher platelet counts and driver mutations in JAK2, CALR or MPL. Thrombotic and hemorrhagic complications are main causes of morbidity/mortality. Platelet functional alterations have been previously reported in patients with ET, also higher reticulated platelet fraction and higher aggregation potential compared to healthy controls.
Aims
To investigate platelet activity and thrombin generation (TG) in patients with ET with different molecular mutations.
Methods
Twenty-two adult patients with ET according to 2017 WHO classification and 10 healthy controls were included. Patients did not receive cytoreductive treatment, and antiaggregant drugs were stopped 7 days prior to sample collection. Patients group included JAK2 mutations (n=11), CALR (n=3), MPL (n=1) and triple-negative (TN)(n=5). Platelet characteristics and functional assessment included flow cytometry and TGT using Calibrated Automated Thrombogram (CAT) using PPP-low as trigger.
Results
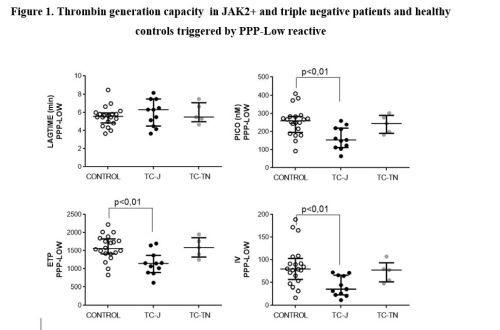
ET patients included 21 females and 1 male with median age of 51 years (24-76). Median platelet count was 631 x109/L (245-1102) and median platelet volume was 8,3fL (7,2-10,8). Fibrinogen receptors on platelets from JAK2+ patients had decreased capacity to be activation by agonists TRAP (p<0.01) and ADP (p<0.01). Platelets from JAK2+ and TN patients exposed P-selectin levels similar to controls after agonist stimulation. Decreased CD63 exposure was noted on JAK2+ group after TRAP stimulation (p<0.05).No significant differences in vWF receptor expression were detected among groups. Plasma from JAK2+ patients had less thrombogenic potential according to the reduced values of endogenous thrombin potential (ETP) (p<0.01),peak (p=0.01) and Velocity index (VI) (p=<0,01) (Figure 1). Platelets from patients with MPL mutation had less fibrinogen receptors with reduced capacity to be activated by TRAP and ADP. All evaluated activation markers were decreased in CALR+ platelets. In MPL+, basal exposure of P-selectin and of CD63 were increased compared to controls. vWF receptor level in CALR+ and MPL+ was similar to controls. TG capacity in CALR+ showed decrease in ETP, peak and VI similar to findings in JAK2+. In phospholipid-dependent TG, diminished ETP and activation index was observed in CALR+. TG depending on tissue factor on microparticles was similar to controls in CALR+.
Conclusion
Our results suggest that molecular profile in ET patients may influence platelet activity and TG. Some alterations were also found in CALR+ and MPL+ patients, but due to the small number of patients it´s no possible to conclude a characteristic pattern in these patients Studies increasing number of patients included should be performed to identify a characteristic pattern of haemostasis and coagulation for each mutation that could help to adjust antiaggregant treatment in ET patients.
Keyword(s): Essential Thrombocytemia, Myeloproliferative disorder, Platelet activation, Thrombin generation
Abstract: EP1072
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Biology & Translational Research
Background
Myeloproliferative neoplasms (MPNs) like Essential Thrombocythemia (ET) presents with higher platelet counts and driver mutations in JAK2, CALR or MPL. Thrombotic and hemorrhagic complications are main causes of morbidity/mortality. Platelet functional alterations have been previously reported in patients with ET, also higher reticulated platelet fraction and higher aggregation potential compared to healthy controls.
Aims
To investigate platelet activity and thrombin generation (TG) in patients with ET with different molecular mutations.
Methods
Twenty-two adult patients with ET according to 2017 WHO classification and 10 healthy controls were included. Patients did not receive cytoreductive treatment, and antiaggregant drugs were stopped 7 days prior to sample collection. Patients group included JAK2 mutations (n=11), CALR (n=3), MPL (n=1) and triple-negative (TN)(n=5). Platelet characteristics and functional assessment included flow cytometry and TGT using Calibrated Automated Thrombogram (CAT) using PPP-low as trigger.
Results
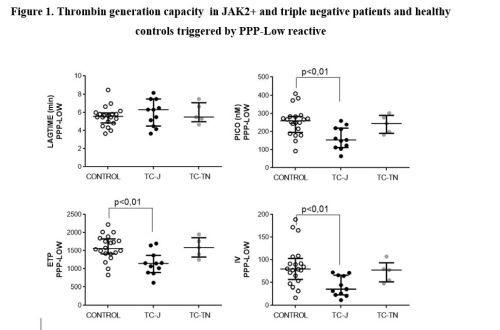
ET patients included 21 females and 1 male with median age of 51 years (24-76). Median platelet count was 631 x109/L (245-1102) and median platelet volume was 8,3fL (7,2-10,8). Fibrinogen receptors on platelets from JAK2+ patients had decreased capacity to be activation by agonists TRAP (p<0.01) and ADP (p<0.01). Platelets from JAK2+ and TN patients exposed P-selectin levels similar to controls after agonist stimulation. Decreased CD63 exposure was noted on JAK2+ group after TRAP stimulation (p<0.05).No significant differences in vWF receptor expression were detected among groups. Plasma from JAK2+ patients had less thrombogenic potential according to the reduced values of endogenous thrombin potential (ETP) (p<0.01),peak (p=0.01) and Velocity index (VI) (p=<0,01) (Figure 1). Platelets from patients with MPL mutation had less fibrinogen receptors with reduced capacity to be activated by TRAP and ADP. All evaluated activation markers were decreased in CALR+ platelets. In MPL+, basal exposure of P-selectin and of CD63 were increased compared to controls. vWF receptor level in CALR+ and MPL+ was similar to controls. TG capacity in CALR+ showed decrease in ETP, peak and VI similar to findings in JAK2+. In phospholipid-dependent TG, diminished ETP and activation index was observed in CALR+. TG depending on tissue factor on microparticles was similar to controls in CALR+.
Conclusion
Our results suggest that molecular profile in ET patients may influence platelet activity and TG. Some alterations were also found in CALR+ and MPL+ patients, but due to the small number of patients it´s no possible to conclude a characteristic pattern in these patients Studies increasing number of patients included should be performed to identify a characteristic pattern of haemostasis and coagulation for each mutation that could help to adjust antiaggregant treatment in ET patients.
Keyword(s): Essential Thrombocytemia, Myeloproliferative disorder, Platelet activation, Thrombin generation


