
Contributions
Abstract: EP1049
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
Multiple myeloma (MM) remains incurable and relapses are common despite new treatment options. Most patients eventually progress despite an increasing armamentarium of anti-myeloma drugs such as proteasome inhibitors (PIs), immunomodulatory drugs (IMiDs), and anti-CD38 monoclonal antibodies. Recycling of previous treatment regimens is often the only alternative available for these patients, which highlights the need for new drug targets and treatment options. The chimeric antigen receptor (CAR) T-cell therapy ciltacabtagene autoleucel (cilta-cel; JNJ-68284528) has two BCMA–targeting single-domain antibodies designed to confer avidity. Initial results from the phase 1b/2 CARTITUDE-1 study (NCT03548207) have shown that a single infusion of cilta-cel yielded early, deep, and durable responses with a manageable safety profile in patients with heavily pretreated RRMM. To date, cilta-cel has not been directly compared with other therapies in development for RRMM in clinical trials. A systematic literature review using PRISMA guidelines identified selinexor + dexamethasone as a potential non-BCMA-targeting comparator in the triple-class exposed RRMM patient population.
Aims
To compare efficacy outcomes in patients who received cilta-cel in CARTITUDE-1 to those who received selinexor + dexamethasone in the STORM trial (Part 2; NCT02336815).
Methods
CARTITUDE-1 included triple-class exposed patients who received ≥3 prior lines of therapy or were double refractory to an IMiD and PI, had ECOG score of ≤1, and disease progression ≤12 months after the last line of therapy. Unanchored matching-adjusted indirect treatment (MAIC) comparisons were performed based on individual patient-level data from 97 infused patients in CARTITUDE-1 and published aggregate-level data from STORM Part 2 (N=122). Patients from CARTITUDE-1 (N=73) who matched the eligibility criteria for STORM Part 2 (penta-drug exposed, ≥ triple-class refractory, and refractory to daratumumab and last line of treatment) were included in the analysis. Individual patient data for time-to-event outcomes from STORM Part 2 were simulated based on the published Kaplan-Meier curves. CARTITUDE-1 patients were matched to the modified intent-to-treat population from STORM Part 2 on available prognostic factors identified from the literature and based on clinical expertise using propensity score weighting methods. Outcomes included overall response rate (ORR), complete response or better (≥CR), progression-free survival (PFS), and overall survival (OS). For ORR and ≥CR, the relative effects of cilta-cel versus selinexor + dexamethasone were quantified using odds ratios (OR) and 95% confidence intervals (CI) derived from a weighted logistic regression analysis, while time to event endpoints were analyzed using a weighted Cox proportional hazards model. A similar comparative analysis was performed which included all enrolled patients in CARTITUDE-1.
Results
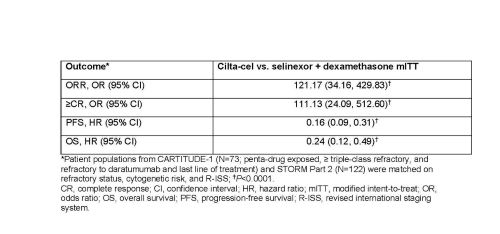
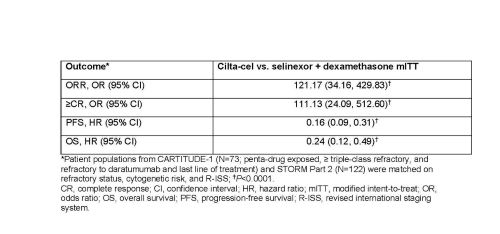
Cilta-cel was associated with statistically significant improvements in ORR, ≥CR, PFS, and OS versus selinexor + dexamethasone in a population matched to STORM Part 2 (Table). Similarly, cilta-cel was associated with higher efficacy in the comparative analysis which included all patients enrolled in CARTITUDE-1.
Conclusion
These analyses demonstrated improved efficacy with cilta-cel versus selinexor + dexamethasone for ORR, ≥CR, PFS, and OS, highlighting its potential in patients with heavily pretreated RRMM.
Keyword(s): B-cell maturation antigen, CAR-T, Multiple myeloma
Abstract: EP1049
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
Multiple myeloma (MM) remains incurable and relapses are common despite new treatment options. Most patients eventually progress despite an increasing armamentarium of anti-myeloma drugs such as proteasome inhibitors (PIs), immunomodulatory drugs (IMiDs), and anti-CD38 monoclonal antibodies. Recycling of previous treatment regimens is often the only alternative available for these patients, which highlights the need for new drug targets and treatment options. The chimeric antigen receptor (CAR) T-cell therapy ciltacabtagene autoleucel (cilta-cel; JNJ-68284528) has two BCMA–targeting single-domain antibodies designed to confer avidity. Initial results from the phase 1b/2 CARTITUDE-1 study (NCT03548207) have shown that a single infusion of cilta-cel yielded early, deep, and durable responses with a manageable safety profile in patients with heavily pretreated RRMM. To date, cilta-cel has not been directly compared with other therapies in development for RRMM in clinical trials. A systematic literature review using PRISMA guidelines identified selinexor + dexamethasone as a potential non-BCMA-targeting comparator in the triple-class exposed RRMM patient population.
Aims
To compare efficacy outcomes in patients who received cilta-cel in CARTITUDE-1 to those who received selinexor + dexamethasone in the STORM trial (Part 2; NCT02336815).
Methods
CARTITUDE-1 included triple-class exposed patients who received ≥3 prior lines of therapy or were double refractory to an IMiD and PI, had ECOG score of ≤1, and disease progression ≤12 months after the last line of therapy. Unanchored matching-adjusted indirect treatment (MAIC) comparisons were performed based on individual patient-level data from 97 infused patients in CARTITUDE-1 and published aggregate-level data from STORM Part 2 (N=122). Patients from CARTITUDE-1 (N=73) who matched the eligibility criteria for STORM Part 2 (penta-drug exposed, ≥ triple-class refractory, and refractory to daratumumab and last line of treatment) were included in the analysis. Individual patient data for time-to-event outcomes from STORM Part 2 were simulated based on the published Kaplan-Meier curves. CARTITUDE-1 patients were matched to the modified intent-to-treat population from STORM Part 2 on available prognostic factors identified from the literature and based on clinical expertise using propensity score weighting methods. Outcomes included overall response rate (ORR), complete response or better (≥CR), progression-free survival (PFS), and overall survival (OS). For ORR and ≥CR, the relative effects of cilta-cel versus selinexor + dexamethasone were quantified using odds ratios (OR) and 95% confidence intervals (CI) derived from a weighted logistic regression analysis, while time to event endpoints were analyzed using a weighted Cox proportional hazards model. A similar comparative analysis was performed which included all enrolled patients in CARTITUDE-1.
Results
Cilta-cel was associated with statistically significant improvements in ORR, ≥CR, PFS, and OS versus selinexor + dexamethasone in a population matched to STORM Part 2 (Table). Similarly, cilta-cel was associated with higher efficacy in the comparative analysis which included all patients enrolled in CARTITUDE-1.
Conclusion
These analyses demonstrated improved efficacy with cilta-cel versus selinexor + dexamethasone for ORR, ≥CR, PFS, and OS, highlighting its potential in patients with heavily pretreated RRMM.
Keyword(s): B-cell maturation antigen, CAR-T, Multiple myeloma


