
Contributions
Abstract: EP1040
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
Bone marrow (peripheral blood stem cells (PBSCs)) autologous transplantation is the standard care for transplant-eligible patients with multiple myeloma. This treatment option is somewhat limited due to the high consumption of economic resources and the access to Cryobank. We performed a retrospective analysis of multiple myeloma patients who underwent autologous transplantation using non-cryopreserved and сryopreserved grafts at our institution from March 2016 to April 2020.
Aims
Compare the results of autologous transplantation using non-cryopreserved and cryopreserved hematopoietic stem cells (HSC).
Methods
78 patients with MM were included in the study (male/female ratio 1.3:1).
All patients got the standard immunochemotherapy programs. They had remission (≥partial response) till the auto-HSCT. Patients were divided in two groups depending on the technique of HSC storage: non-CRYO (n=35) and CRYO (n=43). Cryopreservation is a standard method of storage of HSC suspension. In our work we used the native HSC suspension which was saved from +4 °C to +6 °C during 72 hours.
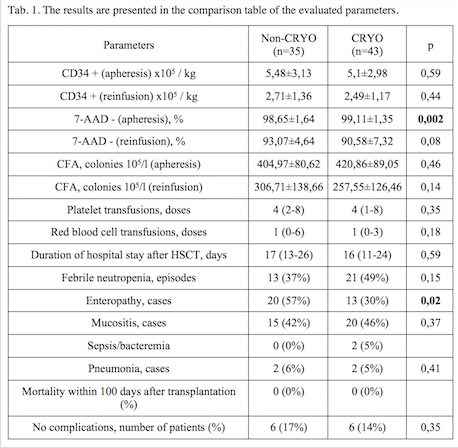
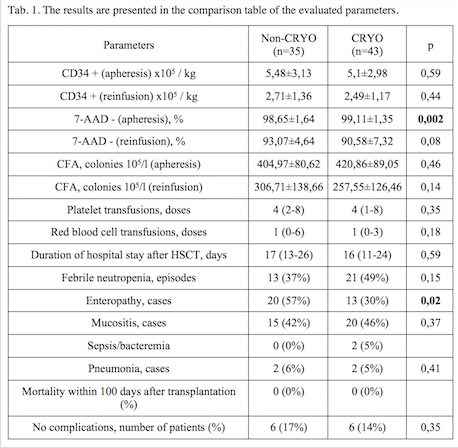
An effectivity and safety were evaluated in such parameters as the number of CD34+ and 7AAD- cells, colony-forming ability (CFA). All of these were made after apheresis and before reinfusion of HSC.
Additionally, the effectiveness of therapy was assessed according to the IMWG and MRD response criteria before SCT and on day +100.
Results
There were no differences in the total number of CD34 + cells x 106/kg, or in the level of 7AAD– cells, or in the total CFA. However, there was a significant difference in the percentage of loss of CD34+ cells from the moment of apheresis to the moment of reinfusion. We suppose it was caused adverse effects by temperature changes in CRYO group. In both groups, there were no severe infusion reactions on day 0. The adverse events were absent in the non-CRYO group. But 29/43 (67.4%) patients had such symptoms in the CRYO group on day 0 (nausea and vomiting – 7 patients (16,3%), tachycardia – 16 patients (37,2%), stenocardia – 3 patients (7,0%), arterial hypertension – 6 patients (13,9%), increased total bilirubin and indicator liver enzymes – 5 patients (11,6%)).
All patients had full recovery of hematopoiesis till discharge from the hospital. Neutrophil recovery was achieved at 11th day (range 9-14) and platelets at 12th day (range 8-19) in the non-CRYO group, and 10th day (range 8-14) and 12th day (range 8 -20) in the CRYO group, respectively.
The frequency of achieving a partial response before autoHSCT was 37% (13/35), a very good partial response - 40% (14/35), a complete response - 23% (8/35) in the non-CRYO group and 72% (31/43), 14% (6/43) and 14% (6/43) in the CRIO group, respectively. HSCT was improved the efficiency of treatment as well as the frequency of complete and MRD-negative responses in both groups. Partial response after autoHSCT was achieved in 23% (8/35) patients, very good partial response in 40% (14/35), complete response in 37% (13/35) in the non-CRYO group compared to the CRYO group (47% (20/43), 21% (9/43) and 32% (14/43), respectively).
The MRD status was assessed before and after autoHSCT in 48 patients. The frequency of MRD-negative response before autoHSCT was 37,5%, after transplantation – 54,5% in the non-CRYO group and 16% and 33% in the CRYO group, respectively.
Conclusion
The method of storage of PBSCs without cryopreserved is equal to traditional method controlled freezing with Dimethyl sulfoxide and can be used in hospitals which have no a Cryobank in their composition.
Keyword(s): Myeloma, Stem cell transplant, Transplant
Abstract: EP1040
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
Bone marrow (peripheral blood stem cells (PBSCs)) autologous transplantation is the standard care for transplant-eligible patients with multiple myeloma. This treatment option is somewhat limited due to the high consumption of economic resources and the access to Cryobank. We performed a retrospective analysis of multiple myeloma patients who underwent autologous transplantation using non-cryopreserved and сryopreserved grafts at our institution from March 2016 to April 2020.
Aims
Compare the results of autologous transplantation using non-cryopreserved and cryopreserved hematopoietic stem cells (HSC).
Methods
78 patients with MM were included in the study (male/female ratio 1.3:1).
All patients got the standard immunochemotherapy programs. They had remission (≥partial response) till the auto-HSCT. Patients were divided in two groups depending on the technique of HSC storage: non-CRYO (n=35) and CRYO (n=43). Cryopreservation is a standard method of storage of HSC suspension. In our work we used the native HSC suspension which was saved from +4 °C to +6 °C during 72 hours.
An effectivity and safety were evaluated in such parameters as the number of CD34+ and 7AAD- cells, colony-forming ability (CFA). All of these were made after apheresis and before reinfusion of HSC.
Additionally, the effectiveness of therapy was assessed according to the IMWG and MRD response criteria before SCT and on day +100.
Results
There were no differences in the total number of CD34 + cells x 106/kg, or in the level of 7AAD– cells, or in the total CFA. However, there was a significant difference in the percentage of loss of CD34+ cells from the moment of apheresis to the moment of reinfusion. We suppose it was caused adverse effects by temperature changes in CRYO group. In both groups, there were no severe infusion reactions on day 0. The adverse events were absent in the non-CRYO group. But 29/43 (67.4%) patients had such symptoms in the CRYO group on day 0 (nausea and vomiting – 7 patients (16,3%), tachycardia – 16 patients (37,2%), stenocardia – 3 patients (7,0%), arterial hypertension – 6 patients (13,9%), increased total bilirubin and indicator liver enzymes – 5 patients (11,6%)).
All patients had full recovery of hematopoiesis till discharge from the hospital. Neutrophil recovery was achieved at 11th day (range 9-14) and platelets at 12th day (range 8-19) in the non-CRYO group, and 10th day (range 8-14) and 12th day (range 8 -20) in the CRYO group, respectively.
The frequency of achieving a partial response before autoHSCT was 37% (13/35), a very good partial response - 40% (14/35), a complete response - 23% (8/35) in the non-CRYO group and 72% (31/43), 14% (6/43) and 14% (6/43) in the CRIO group, respectively. HSCT was improved the efficiency of treatment as well as the frequency of complete and MRD-negative responses in both groups. Partial response after autoHSCT was achieved in 23% (8/35) patients, very good partial response in 40% (14/35), complete response in 37% (13/35) in the non-CRYO group compared to the CRYO group (47% (20/43), 21% (9/43) and 32% (14/43), respectively).
The MRD status was assessed before and after autoHSCT in 48 patients. The frequency of MRD-negative response before autoHSCT was 37,5%, after transplantation – 54,5% in the non-CRYO group and 16% and 33% in the CRYO group, respectively.
Conclusion
The method of storage of PBSCs without cryopreserved is equal to traditional method controlled freezing with Dimethyl sulfoxide and can be used in hospitals which have no a Cryobank in their composition.
Keyword(s): Myeloma, Stem cell transplant, Transplant


