
Contributions
Abstract: EP1035
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
National registers including all multiple myeloma (MM) patients can give fast information on the implementation and effect of new treatment strategies. In Denmark ans Sweden MM patients have been registered at diagnosis of MM since 2005 and 2008, respectively. Data in characteristics, treatment and outcome is collected and the coverage is close to 100% coverage.
Aims
By merging the national databases in Sweden and Denmark where drug access and treatment guidelines are comparable and MM care universal, we study the implementation of guidelines and the effect of treatments in the real world.
Methods
We present treatment data from 10.062 patients annotated in the Danish Multiple Myeloma Registry (DMMR; n=4177) in the calendar period 2005 to 2018 and the Swedish Myeloma registry (SMR; n=5885) in the calendar period 2008-2018. Induction treatments for patients undergoing high-dose melphalan and autologous stem cell transplant, and first line treatment for patients with non-HDM/ASCT is presented.
Results
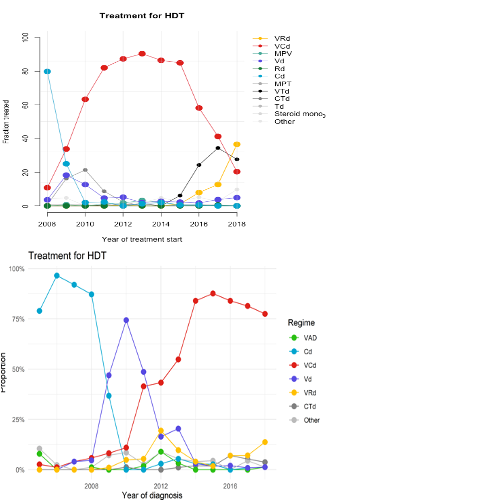
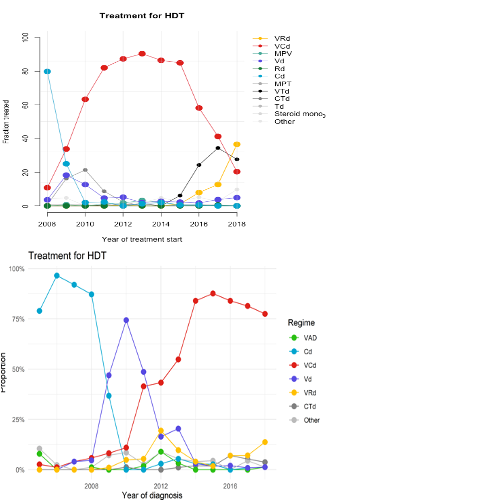
In both countries, 30% of newly diagnosed patients received HDM/ASCT upfront. Figure 1 A (above) and B (below) illustrate the use of induction treatment preceding HDT/ASCT for 1791 in Sweden, and 1281 patients in Denmark, respectively. Before 2010, induction treatment consisted of two-drug combinations of either cyclophosphamide/dexamethasone (Cydex) or bortezomib/dexamethasone (Vd) in both countries. Later, the 3-drug combination bortezomib/cyclophosphamide/dexamethasone (VCD) soon became a commonly used induction treatment. From 2015 an increasing proportion received 3-drug combinations containing an immunomodulatory drug (IMiD), a proteasome inhibitor (PI) and dexamethasone. In 2017-2018, the proportion of patients receiving induction treatment with VCD, thalidomide combinations and VRD was 79.8 %, 4.7% and 9.8 % in Denmark and VCD, VTd and VRD 32%, 32%, and 22% in Sweden, respectively.
In elderly patients, the use of 2-drug alkylator-based regimens melphalan/prednisone (MP) in Sweden and MP or CyDex in Denmark gradually shifted towards 2- or 3-drug combinations with an IMiD or a PI. In Sweden the use of MP decreased from 50 % in 2008 to 5 % in 2017-2018 and was replaced first by the combination of melphalan/thalidomide/prednisone (MPT) and later by melphalan/bortezomib/prednisone (MPV). In Denmark, a similar decrease in the use of MP was observed with a shift from MP to MPT followed by MPV. After 2015 an increasing proportion in both countries were treated with the combinations Vd and VCD while the use of lenalidomide-based combinations differed, with more patients treated with VRd in Denmark. In 2017-2018 the proportion of elderly patients treated with VD, VCD, Rd or VRD in 1st line were 13.1%, 20.7%, 8.7%, 15.0% in Denmark and 21%, 11%, 10%, and 7% in Sweden, respectively.
In the DMMR we show an increase in 5-year OS in patients ≤65 year from 59.8% in the calendar period 2008-2013 to 73.4% in the calendar period 2014-2019. In the same calendar periods an increase in 5-years OS was also noted for patients > 65 years from 27.5% (2008-2013) to 39.8% (2014-2019)(www.myeloma.dk). Similarly, in the SMR, in all patients diagnosed 2008-2019, the 5-year OS is now reaching 70% in patients ≤65 and 35% in patients >65 years (www.cancercentrum.se/Årsrapport2020).
Conclusion
National registries that include all MM patients are an important source of knowledge on treatment and outcome. Our data show that new treatment strategies are rapidly implemented in both countries in parallel with increased OS for all patient groups.
Keyword(s): Multiple myeloma, Population, Survival, Treatment
Abstract: EP1035
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
National registers including all multiple myeloma (MM) patients can give fast information on the implementation and effect of new treatment strategies. In Denmark ans Sweden MM patients have been registered at diagnosis of MM since 2005 and 2008, respectively. Data in characteristics, treatment and outcome is collected and the coverage is close to 100% coverage.
Aims
By merging the national databases in Sweden and Denmark where drug access and treatment guidelines are comparable and MM care universal, we study the implementation of guidelines and the effect of treatments in the real world.
Methods
We present treatment data from 10.062 patients annotated in the Danish Multiple Myeloma Registry (DMMR; n=4177) in the calendar period 2005 to 2018 and the Swedish Myeloma registry (SMR; n=5885) in the calendar period 2008-2018. Induction treatments for patients undergoing high-dose melphalan and autologous stem cell transplant, and first line treatment for patients with non-HDM/ASCT is presented.
Results
In both countries, 30% of newly diagnosed patients received HDM/ASCT upfront. Figure 1 A (above) and B (below) illustrate the use of induction treatment preceding HDT/ASCT for 1791 in Sweden, and 1281 patients in Denmark, respectively. Before 2010, induction treatment consisted of two-drug combinations of either cyclophosphamide/dexamethasone (Cydex) or bortezomib/dexamethasone (Vd) in both countries. Later, the 3-drug combination bortezomib/cyclophosphamide/dexamethasone (VCD) soon became a commonly used induction treatment. From 2015 an increasing proportion received 3-drug combinations containing an immunomodulatory drug (IMiD), a proteasome inhibitor (PI) and dexamethasone. In 2017-2018, the proportion of patients receiving induction treatment with VCD, thalidomide combinations and VRD was 79.8 %, 4.7% and 9.8 % in Denmark and VCD, VTd and VRD 32%, 32%, and 22% in Sweden, respectively.
In elderly patients, the use of 2-drug alkylator-based regimens melphalan/prednisone (MP) in Sweden and MP or CyDex in Denmark gradually shifted towards 2- or 3-drug combinations with an IMiD or a PI. In Sweden the use of MP decreased from 50 % in 2008 to 5 % in 2017-2018 and was replaced first by the combination of melphalan/thalidomide/prednisone (MPT) and later by melphalan/bortezomib/prednisone (MPV). In Denmark, a similar decrease in the use of MP was observed with a shift from MP to MPT followed by MPV. After 2015 an increasing proportion in both countries were treated with the combinations Vd and VCD while the use of lenalidomide-based combinations differed, with more patients treated with VRd in Denmark. In 2017-2018 the proportion of elderly patients treated with VD, VCD, Rd or VRD in 1st line were 13.1%, 20.7%, 8.7%, 15.0% in Denmark and 21%, 11%, 10%, and 7% in Sweden, respectively.
In the DMMR we show an increase in 5-year OS in patients ≤65 year from 59.8% in the calendar period 2008-2013 to 73.4% in the calendar period 2014-2019. In the same calendar periods an increase in 5-years OS was also noted for patients > 65 years from 27.5% (2008-2013) to 39.8% (2014-2019)(www.myeloma.dk). Similarly, in the SMR, in all patients diagnosed 2008-2019, the 5-year OS is now reaching 70% in patients ≤65 and 35% in patients >65 years (www.cancercentrum.se/Årsrapport2020).
Conclusion
National registries that include all MM patients are an important source of knowledge on treatment and outcome. Our data show that new treatment strategies are rapidly implemented in both countries in parallel with increased OS for all patient groups.
Keyword(s): Multiple myeloma, Population, Survival, Treatment


