
Contributions
Abstract: EP1032
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
Gain in chromosome 1q (+1q) is one of the most common recurrent cytogenetic abnormalities in multiple myeloma (MM). Previous studies indicate an association with inferior outcomes, but there is uncertainty about the prognostic impact of this abnormality relative to other high risk cytogenetic abnormalities (HRCAs).
Aims
To evaluate clinical characteristics, response to treatment and survival outcomes in newly diagnosed transplant-eligible MM patients (pts) with +1q
Methods
Single centre retrospective study including newly diagnosed transplant-eligible MM pts treated between January 2012 and December 2020, who had cytogenetic analysis by fluorescence in situ hybridization (FISH) performed at diagnosis. FISH abnormalities included +1q, del17p, t(11;14), t(4;14), t(14;16) and hyperdiploidy. +1q was defined by ≥3 copies of CKS1B locus (1q21), with a threshold of 3-5%. Clinical data were obtained by review of electronic medical records. Response evaluation was according to the International Myeloma Working Group (IMWG) criteria. HRCAs as defined by the Revised-International Staging System (R-ISS): del17p, t(4;14) and/or t(14;16).
Results
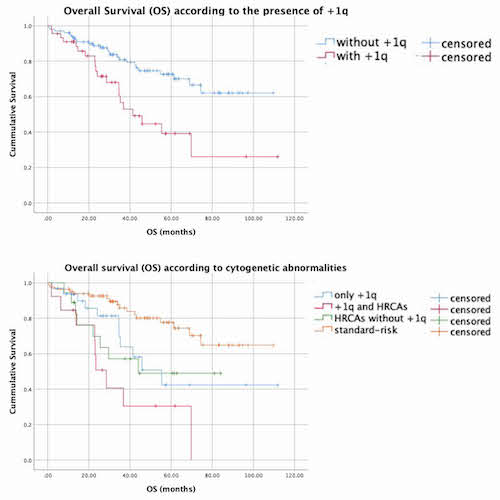
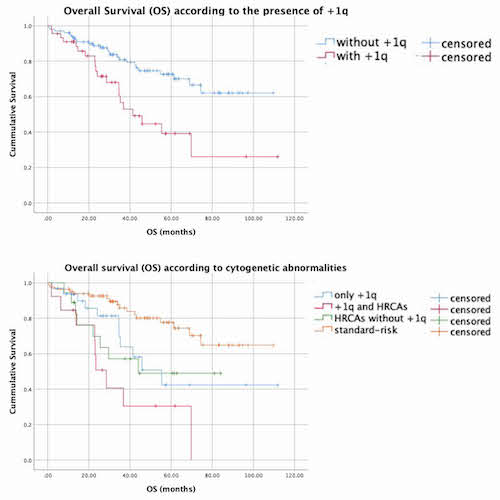
This cohort included 150 pts, with a median age of 60 years (range 35-72); 53.3% were male. 30.6% of the pts had documented +1q and 20.8% expressed HRCAs. All patients received bortezomib-based induction regimens, 42.0% in association with an immunomodulatory drug (IMiD) (thalidomide in 25.3% of the pts, lenalidomide in 16.7%), 52.0% with an alkylating agent and 4.0% with an anthracycline, followed by single autologous stem-cell transplantation (ASCT) in 74.0% and tandem ASCT in 16.0%. Median follow-up (FU) was 34.6 months (mo). Baseline clinical characteristics were similar in pts with +1q (gr 1) and without +1q (gr 2). There were also no differences in overall response rates to induction therapy between gr 1 and 2 (93.3% vs 89.9%; p=0.37). Overall survival (OS) and progression free survival (PFS) were compared between gr 1 and 2, and four other subgroups: standard risk cytogenetics (gr 3), presence of +1q alone (gr 4), presence of ≥1 HRCAs (gr 5) and presence of +1q and ≥1 HRCAs (gr 6). At median FU, OS was significantly lower in gr 1 compared with gr 2 (60.5% vs. 82.3%; p= 0.001), as was PFS (24.6% vs. 56.8%; p<0.001). OS was also lower in gr 4, 5 and 6, when compared with gr 3 [69.8% (vs 87.7%; p=0.019), 57.1% (vs. 87.7%; p<0.01) and 40.6% (vs. 87.7%; p=0.02), respectively], as well as PFS [23.0% (vs 67.0% p<0.001), 23.4% (vs. 67.0%; p=0.011) and 34.4% (vs. 67.0% p=0.032), respectively]. When comparing gr 1 and 2 according to induction regimen (IMiD vs non-IMiD), there was lower OS in gr 1 (56.0% vs. 80.9%; p=0.003) with non-IMiD-based regimens, but no difference with IMiD-based regimens (76.7% vs. 83.4%; p=0.288). In multivariate Cox-regression analyses including age, presence of HRCAs, presence of +1q, and IMiD-based induction regimens, +1q remained a significant and independent adverse factor for OS [HR 2.46 (95% CI 1.34-4.52); p=0.004] and PFS [2.13 (95% CI 1.34-3.38); p=0.001], whereas HRCAs only significantly impacted OS [3.03 (95% CI 1.61-5.72); p=0.001].
Conclusion
Our results corroborate the high prevalence of +1q in MM, although we found no association with any specific clinical characteristics at diagnosis. +1q had a significant negative impact in OS and PFS. IMiD-based regimens may have a beneficial effect in terms of survival in this subgroup of patients.
Keyword(s): FISH, Imids, Multiple myeloma
Abstract: EP1032
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
Gain in chromosome 1q (+1q) is one of the most common recurrent cytogenetic abnormalities in multiple myeloma (MM). Previous studies indicate an association with inferior outcomes, but there is uncertainty about the prognostic impact of this abnormality relative to other high risk cytogenetic abnormalities (HRCAs).
Aims
To evaluate clinical characteristics, response to treatment and survival outcomes in newly diagnosed transplant-eligible MM patients (pts) with +1q
Methods
Single centre retrospective study including newly diagnosed transplant-eligible MM pts treated between January 2012 and December 2020, who had cytogenetic analysis by fluorescence in situ hybridization (FISH) performed at diagnosis. FISH abnormalities included +1q, del17p, t(11;14), t(4;14), t(14;16) and hyperdiploidy. +1q was defined by ≥3 copies of CKS1B locus (1q21), with a threshold of 3-5%. Clinical data were obtained by review of electronic medical records. Response evaluation was according to the International Myeloma Working Group (IMWG) criteria. HRCAs as defined by the Revised-International Staging System (R-ISS): del17p, t(4;14) and/or t(14;16).
Results
This cohort included 150 pts, with a median age of 60 years (range 35-72); 53.3% were male. 30.6% of the pts had documented +1q and 20.8% expressed HRCAs. All patients received bortezomib-based induction regimens, 42.0% in association with an immunomodulatory drug (IMiD) (thalidomide in 25.3% of the pts, lenalidomide in 16.7%), 52.0% with an alkylating agent and 4.0% with an anthracycline, followed by single autologous stem-cell transplantation (ASCT) in 74.0% and tandem ASCT in 16.0%. Median follow-up (FU) was 34.6 months (mo). Baseline clinical characteristics were similar in pts with +1q (gr 1) and without +1q (gr 2). There were also no differences in overall response rates to induction therapy between gr 1 and 2 (93.3% vs 89.9%; p=0.37). Overall survival (OS) and progression free survival (PFS) were compared between gr 1 and 2, and four other subgroups: standard risk cytogenetics (gr 3), presence of +1q alone (gr 4), presence of ≥1 HRCAs (gr 5) and presence of +1q and ≥1 HRCAs (gr 6). At median FU, OS was significantly lower in gr 1 compared with gr 2 (60.5% vs. 82.3%; p= 0.001), as was PFS (24.6% vs. 56.8%; p<0.001). OS was also lower in gr 4, 5 and 6, when compared with gr 3 [69.8% (vs 87.7%; p=0.019), 57.1% (vs. 87.7%; p<0.01) and 40.6% (vs. 87.7%; p=0.02), respectively], as well as PFS [23.0% (vs 67.0% p<0.001), 23.4% (vs. 67.0%; p=0.011) and 34.4% (vs. 67.0% p=0.032), respectively]. When comparing gr 1 and 2 according to induction regimen (IMiD vs non-IMiD), there was lower OS in gr 1 (56.0% vs. 80.9%; p=0.003) with non-IMiD-based regimens, but no difference with IMiD-based regimens (76.7% vs. 83.4%; p=0.288). In multivariate Cox-regression analyses including age, presence of HRCAs, presence of +1q, and IMiD-based induction regimens, +1q remained a significant and independent adverse factor for OS [HR 2.46 (95% CI 1.34-4.52); p=0.004] and PFS [2.13 (95% CI 1.34-3.38); p=0.001], whereas HRCAs only significantly impacted OS [3.03 (95% CI 1.61-5.72); p=0.001].
Conclusion
Our results corroborate the high prevalence of +1q in MM, although we found no association with any specific clinical characteristics at diagnosis. +1q had a significant negative impact in OS and PFS. IMiD-based regimens may have a beneficial effect in terms of survival in this subgroup of patients.
Keyword(s): FISH, Imids, Multiple myeloma


