
Contributions
Abstract: EP1020
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
The introduction of novel agents and autologous stem cell transplantation improved the population-level survival of patients with multiple myeloma (MM). However, early mortality (EM) remains a major clinical issue. Identification of risk factors of EM may contribute to more rigorous supportive care measures or different therapeutic approaches in patients at risk for EM.
Aims
This population-based study aimed to assess trends in and risk factors of EM among MM patients diagnosed in the Netherlands during a 30-year period.
Methods
All MM patients diagnosed between 1989-2018 were identified in the Netherlands Cancer Registry, with survival follow-up through 2020. Data on primary therapy, i.e. no therapy and anti-neoplastic therapy were available for all patients. Patients were categorized into three calendar periods (1989-1998, 1999-2008, 2009-2018) and four age groups (≤65, 66-70, 71-80, >80 years). The impact of age, sex, period of diagnosis, hospital type at diagnosis, and prior malignancies, for EM was evaluated using uni- and multivariable Cox regression analyses. Moreover, for patients diagnosed in 2014-2018, detailed data on plasma cell percentage, cytogenetic risk, type of M-protein, levels of β2-microglobulin and albumin, as well as presence of thrombocytopenia, hypercalcemia, renal impairment, anemia, and bone lesions, type and number of novel agents (bortezomib, lenalidomide and/or thalidomide) was evaluated. EM was defined as the date from MM diagnosis to all-cause death ≤180 days.
Results
Our analytical cohort included 28,328 MM patients (median age 70 years; 55% males; 88% diagnosed in non-academic centers; 13% prior malignancies). EM for patients ≤65 was 11%, 11%, and 6% (P<0.001) in 1989-1998, 1999-2008, and 2009-2018, respectively. The corresponding proportions for patients aged 66-70 were 19%, 16%, and 8% (P<0.001), for patients 71-80, 25%, 22%, and 15% (P<0.001), and for patients >80, 40%, 41%, and 31% (P<0.001). EM was significantly lower among patients who received anti-neoplastic therapy as compared to patients who did not receive first-line therapy (13% vs. 29%; P<0.001) and EM decreased for both groups over time. When simultaneously adjusted for calendar period, sex, age, hospital type at diagnosis, prior malignancies, and treatment, patients diagnosed in 2009-2018 had a 42% lower risk of mortality as compared with patients diagnosed in 1989-1998 (hazard ratio, 0.58; P<0.001) with an adverse effect of older age, and prior malignancies.
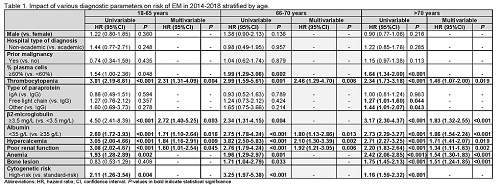
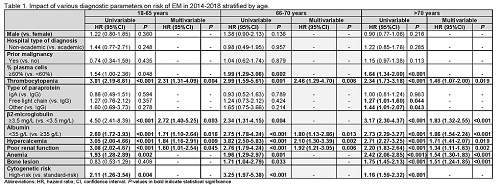
In 2014-2018, 6,380 MM patients were diagnosed of whom 780 (12%) patients died ≤180 days post-diagnosis. For patients ≤70 years, EM was 6% for patients treated with bortezomib, 5% for lenalidomide, 3% for thalidomide as well as for treatment with two novel drugs (P=0.013). EM was similar for patients >70 years treated with bortezomib, lenalidomide, or thalidomide (12%, 15%, 14%, respectively; P=0.441). For patients >70 years treated with a combination of two novel drugs, none died ≤180 days. Albumin <35 g/L, β2-microglobulin ≥3.5 mg/L, thrombocytopenia, hypercalcemia, and poor renal function have an adverse effect on EM for patients ≤70 (Table). In addition, anemia and bone lesions have an adverse effect on EM for patients >70.
Conclusion
In summary, EM among MM patients improved from 1999 onwards. Nevertheless, EM remains high, especially for patients aged >70 years. Patients at risk for EM may benefit from better supportive care or individualized anti-MM therapy.
Keyword(s): Mortality, Multiple myeloma
Abstract: EP1020
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
The introduction of novel agents and autologous stem cell transplantation improved the population-level survival of patients with multiple myeloma (MM). However, early mortality (EM) remains a major clinical issue. Identification of risk factors of EM may contribute to more rigorous supportive care measures or different therapeutic approaches in patients at risk for EM.
Aims
This population-based study aimed to assess trends in and risk factors of EM among MM patients diagnosed in the Netherlands during a 30-year period.
Methods
All MM patients diagnosed between 1989-2018 were identified in the Netherlands Cancer Registry, with survival follow-up through 2020. Data on primary therapy, i.e. no therapy and anti-neoplastic therapy were available for all patients. Patients were categorized into three calendar periods (1989-1998, 1999-2008, 2009-2018) and four age groups (≤65, 66-70, 71-80, >80 years). The impact of age, sex, period of diagnosis, hospital type at diagnosis, and prior malignancies, for EM was evaluated using uni- and multivariable Cox regression analyses. Moreover, for patients diagnosed in 2014-2018, detailed data on plasma cell percentage, cytogenetic risk, type of M-protein, levels of β2-microglobulin and albumin, as well as presence of thrombocytopenia, hypercalcemia, renal impairment, anemia, and bone lesions, type and number of novel agents (bortezomib, lenalidomide and/or thalidomide) was evaluated. EM was defined as the date from MM diagnosis to all-cause death ≤180 days.
Results
Our analytical cohort included 28,328 MM patients (median age 70 years; 55% males; 88% diagnosed in non-academic centers; 13% prior malignancies). EM for patients ≤65 was 11%, 11%, and 6% (P<0.001) in 1989-1998, 1999-2008, and 2009-2018, respectively. The corresponding proportions for patients aged 66-70 were 19%, 16%, and 8% (P<0.001), for patients 71-80, 25%, 22%, and 15% (P<0.001), and for patients >80, 40%, 41%, and 31% (P<0.001). EM was significantly lower among patients who received anti-neoplastic therapy as compared to patients who did not receive first-line therapy (13% vs. 29%; P<0.001) and EM decreased for both groups over time. When simultaneously adjusted for calendar period, sex, age, hospital type at diagnosis, prior malignancies, and treatment, patients diagnosed in 2009-2018 had a 42% lower risk of mortality as compared with patients diagnosed in 1989-1998 (hazard ratio, 0.58; P<0.001) with an adverse effect of older age, and prior malignancies.
In 2014-2018, 6,380 MM patients were diagnosed of whom 780 (12%) patients died ≤180 days post-diagnosis. For patients ≤70 years, EM was 6% for patients treated with bortezomib, 5% for lenalidomide, 3% for thalidomide as well as for treatment with two novel drugs (P=0.013). EM was similar for patients >70 years treated with bortezomib, lenalidomide, or thalidomide (12%, 15%, 14%, respectively; P=0.441). For patients >70 years treated with a combination of two novel drugs, none died ≤180 days. Albumin <35 g/L, β2-microglobulin ≥3.5 mg/L, thrombocytopenia, hypercalcemia, and poor renal function have an adverse effect on EM for patients ≤70 (Table). In addition, anemia and bone lesions have an adverse effect on EM for patients >70.
Conclusion
In summary, EM among MM patients improved from 1999 onwards. Nevertheless, EM remains high, especially for patients aged >70 years. Patients at risk for EM may benefit from better supportive care or individualized anti-MM therapy.
Keyword(s): Mortality, Multiple myeloma


