
Contributions
Abstract: EP1005
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
In recent years, lenalidomide (LEN) has become an increasingly common therapy of multiple myeloma (MM). However, once patients become refractory to LEN, they are generally considered harder to treat, with fewer treatment options available. Real world (RW) evidence on clinical management of LEN-refractory patients is lacking.
Aims
To describe clinical characteristics, treatment patterns, and clinical outcomes across lines of therapy (LoT) in patients who were refractory to LEN therapy for MM.
Methods
Using the Système National des Données de Santé in France, we identified a cohort of adult patients with an initial diagnosis of MM (index date) between Jan 1, 2010–Dec 31, 2018 who received at least one LoT for MM. Within this cohort, patients who were refractory to LEN (defined as having received only 1 LEN-based LoT, with no LEN in any subsequent LoT, and having initiated a new, non-LEN-based treatment regimen within 60 days of the LEN-containing LoT) were assessed. Baseline patient characteristics were captured in the 12 months before index, and symptoms and comorbidities within the 6 months prior to each LoT. The most frequently used regimens following the LEN-refractory LoT were described. Median overall survival (OS), duration of treatment (DoT) and time to next treatment (TTNT) from the start of each LEN-refractory LoT was assessed by Kaplan–Meier method, and 1–5-year landmark survival rates were calculated.
Results
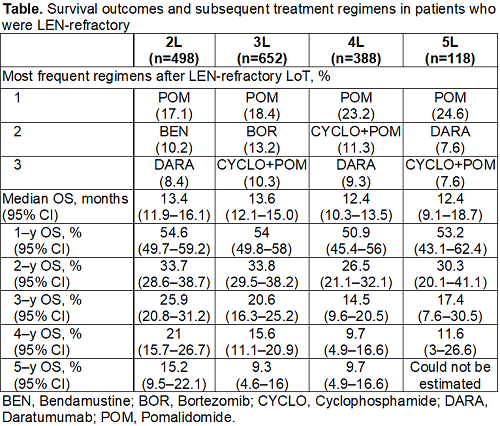
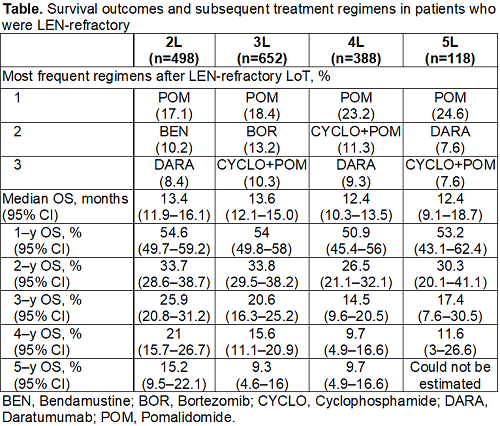
In total, 25,323 patients received ≥1 LoT for MM, of whom 1907 patients were identified as having experienced a LEN-refractory LOT. During the study follow-up period (2010–2018), LEN-based regimens were among the most frequently used regimens in the overall cohort of MM patients, accounting for 14.9% of the 5 most common 1L regimens and 45.7% of the 5 most common 2L regimens. In recent years (2016–2018), LEN-based regimens accounted for 24.7% and 30.6% of the 5 most frequent regimens in 1L and 2L, respectively. Among patients who were refractory to LEN, mean (SD) age was 67.3 (10.7) years at index, and 70.5 (10.5) years when patients became LEN-refractory; 50.9% of LEN-refractory patients were male. Most patients (90.2%) had their LEN-refractory encounter in 2L–4L. The proportion of patients with CRAB symptoms and the median Charlson Comorbidity Index remained consistent across LoTs. After a LEN-refractory LoT, the most frequently used subsequent regimens were generally POM-based (Table). In LEN refractory patients, DoT continued to decrease across LoT (1L: 9.7 months; 2L: 8.4 months; 3L: 6.7 months; 4L: 6.7 months; 5L 7.2 months); similarly, TTNT decreased with advancing LoT (1L–2L: 18.0 months; 2L–3L: 12.0 months; 3L–4L: 9.0 months; 4L–5L: 9.0 months). Survival outcomes in patients following a refractory LEN regimen were poor, with a median OS ranging from 10.4–12.2 months across LoT. Less than a third of patients survived for at least 2 years following a LEN-refractory LoT.
Conclusion
This large, national health database analysis demonstrated that in French RW clinical practice, LEN was frequently used as 1L and 2L therapy for MM, and use of LEN has increased in recent years. After becoming LEN-refractory, patients generally receive POM-based therapy. However, survival outcomes after LEN-refractory regimens were poor, with median survival of around a year and few patients surviving beyond 2 years, regardless of the LEN-refractory LoT. These observations highlight the need for new, efficacious LEN-free treatment options for this hard-to-treat patient population.
Keyword(s): Multiple myeloma, Refractory
Abstract: EP1005
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
In recent years, lenalidomide (LEN) has become an increasingly common therapy of multiple myeloma (MM). However, once patients become refractory to LEN, they are generally considered harder to treat, with fewer treatment options available. Real world (RW) evidence on clinical management of LEN-refractory patients is lacking.
Aims
To describe clinical characteristics, treatment patterns, and clinical outcomes across lines of therapy (LoT) in patients who were refractory to LEN therapy for MM.
Methods
Using the Système National des Données de Santé in France, we identified a cohort of adult patients with an initial diagnosis of MM (index date) between Jan 1, 2010–Dec 31, 2018 who received at least one LoT for MM. Within this cohort, patients who were refractory to LEN (defined as having received only 1 LEN-based LoT, with no LEN in any subsequent LoT, and having initiated a new, non-LEN-based treatment regimen within 60 days of the LEN-containing LoT) were assessed. Baseline patient characteristics were captured in the 12 months before index, and symptoms and comorbidities within the 6 months prior to each LoT. The most frequently used regimens following the LEN-refractory LoT were described. Median overall survival (OS), duration of treatment (DoT) and time to next treatment (TTNT) from the start of each LEN-refractory LoT was assessed by Kaplan–Meier method, and 1–5-year landmark survival rates were calculated.
Results
In total, 25,323 patients received ≥1 LoT for MM, of whom 1907 patients were identified as having experienced a LEN-refractory LOT. During the study follow-up period (2010–2018), LEN-based regimens were among the most frequently used regimens in the overall cohort of MM patients, accounting for 14.9% of the 5 most common 1L regimens and 45.7% of the 5 most common 2L regimens. In recent years (2016–2018), LEN-based regimens accounted for 24.7% and 30.6% of the 5 most frequent regimens in 1L and 2L, respectively. Among patients who were refractory to LEN, mean (SD) age was 67.3 (10.7) years at index, and 70.5 (10.5) years when patients became LEN-refractory; 50.9% of LEN-refractory patients were male. Most patients (90.2%) had their LEN-refractory encounter in 2L–4L. The proportion of patients with CRAB symptoms and the median Charlson Comorbidity Index remained consistent across LoTs. After a LEN-refractory LoT, the most frequently used subsequent regimens were generally POM-based (Table). In LEN refractory patients, DoT continued to decrease across LoT (1L: 9.7 months; 2L: 8.4 months; 3L: 6.7 months; 4L: 6.7 months; 5L 7.2 months); similarly, TTNT decreased with advancing LoT (1L–2L: 18.0 months; 2L–3L: 12.0 months; 3L–4L: 9.0 months; 4L–5L: 9.0 months). Survival outcomes in patients following a refractory LEN regimen were poor, with a median OS ranging from 10.4–12.2 months across LoT. Less than a third of patients survived for at least 2 years following a LEN-refractory LoT.
Conclusion
This large, national health database analysis demonstrated that in French RW clinical practice, LEN was frequently used as 1L and 2L therapy for MM, and use of LEN has increased in recent years. After becoming LEN-refractory, patients generally receive POM-based therapy. However, survival outcomes after LEN-refractory regimens were poor, with median survival of around a year and few patients surviving beyond 2 years, regardless of the LEN-refractory LoT. These observations highlight the need for new, efficacious LEN-free treatment options for this hard-to-treat patient population.
Keyword(s): Multiple myeloma, Refractory


