
Contributions
Abstract: S313
Type: Oral Presentation
Session title: Patient's voice and health outcomes in hematology
Background
Patients with acute myeloid leukemia (AML) who have received a hematopoietic stem cell transplant (HSCT) may consider post-HSCT maintenance therapy to prolong remission. Since there are no universally accepted standard maintenance therapies, patients and physicians need to weigh the risks and benefits of each potential regimen when making treatment decisions. A better understanding of the differences in how patients and physicians each weigh the value of various treatment attributes, and whether either group’s preferences affect the other’s, would be of value in understanding why various treatments are selected.
Aims
To quantify patients’ and physicians’ preferences for post-HSCT AML maintenance treatment.
Methods
A targeted literature review and one-on-one patient (n=6) and physician (n=4) phone interviews informed the post-HSCT AML maintenance treatment attributes used in this discrete choice experiment (DCE). Attribute levels were selected to reflect the range of maintenance treatments available for post-HSCT patients. Patients with AML who had received HSCT and physicians who treat patients with AML in the US, UK, Canada, and Australia were recruited from physician panels to complete a web-based DCE. The DCE participants were presented choice cards each showing a pair of hypothetical treatment profiles with six attributes (chance of 2-year relapse-free survival [RFS], average quality of life [QoL], risk of serious infections, risk of nausea, chance of achieving transfusion independence, and duration of hospitalization per year) of varying levels and asked to choose a preferred treatment per card. This preliminary analysis used conditional logit regression models to estimate preference weights and analyze the impact of treatment attributes on participants’ post-HSCT maintenance therapy treatment choices.
Results
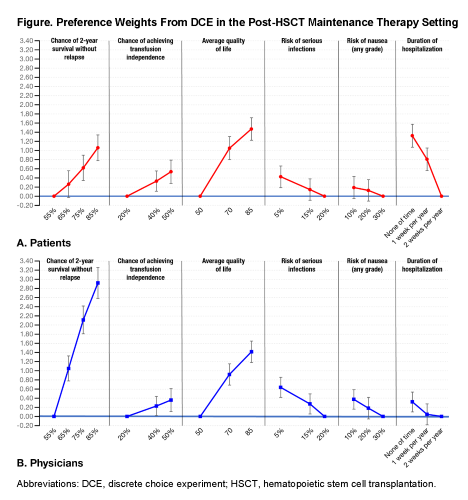
A total of 78 patients with AML post-HSCT (US, n=46; UK, n=30; Canada, n=2) and 145 physicians who treat this population (US, n=48; UK, n=52; Canada, n=29; Australia, n=16) completed the DCE. For patients, average QoL was the most important treatment attribute for post-HSCT maintenance therapy based on preference weights, followed by duration of hospitalization and chance of 2-year RFS (Figure A). Post-HSCT patients were willing to accept a less effective treatment if it reduced hospital stay or improved QoL: the benefit of a 2-week reduction in hospitalization per year or an improvement of QoL by 35 on a 0-100 scale each compensated for a 30% reduction in 2-year RFS. For physicians, chance of 2-year RFS was the most important treatment attribute, followed by average QoL and risk of serious infections (Figure B). Physicians valued duration of hospitalization and chance of achieving transfusion independence less when selecting treatments. Responses from physicians suggested that a 2-week reduction in hospitalization per year could compensate for having to bear an additional 5% risk of serious infection or 10% risk of nausea.
Conclusion
Differences in treatment attribute importance for post-HSCT maintenance therapy were observed between patients and physicians. The DCE results highlight the value patients place on treatments that improve their QoL and reduce the duration of hospitalization. Physicians also valued patients’ QoL when making treatment decisions, so informing physicians of patients’ preferences may influence their choices regarding treatments that better meet patients’ needs and improve patients’ treatment satisfaction.
Keyword(s): Quality of life, Treatment
Abstract: S313
Type: Oral Presentation
Session title: Patient's voice and health outcomes in hematology
Background
Patients with acute myeloid leukemia (AML) who have received a hematopoietic stem cell transplant (HSCT) may consider post-HSCT maintenance therapy to prolong remission. Since there are no universally accepted standard maintenance therapies, patients and physicians need to weigh the risks and benefits of each potential regimen when making treatment decisions. A better understanding of the differences in how patients and physicians each weigh the value of various treatment attributes, and whether either group’s preferences affect the other’s, would be of value in understanding why various treatments are selected.
Aims
To quantify patients’ and physicians’ preferences for post-HSCT AML maintenance treatment.
Methods
A targeted literature review and one-on-one patient (n=6) and physician (n=4) phone interviews informed the post-HSCT AML maintenance treatment attributes used in this discrete choice experiment (DCE). Attribute levels were selected to reflect the range of maintenance treatments available for post-HSCT patients. Patients with AML who had received HSCT and physicians who treat patients with AML in the US, UK, Canada, and Australia were recruited from physician panels to complete a web-based DCE. The DCE participants were presented choice cards each showing a pair of hypothetical treatment profiles with six attributes (chance of 2-year relapse-free survival [RFS], average quality of life [QoL], risk of serious infections, risk of nausea, chance of achieving transfusion independence, and duration of hospitalization per year) of varying levels and asked to choose a preferred treatment per card. This preliminary analysis used conditional logit regression models to estimate preference weights and analyze the impact of treatment attributes on participants’ post-HSCT maintenance therapy treatment choices.
Results
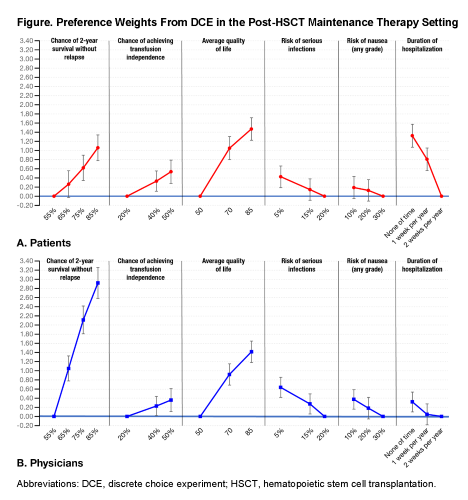
A total of 78 patients with AML post-HSCT (US, n=46; UK, n=30; Canada, n=2) and 145 physicians who treat this population (US, n=48; UK, n=52; Canada, n=29; Australia, n=16) completed the DCE. For patients, average QoL was the most important treatment attribute for post-HSCT maintenance therapy based on preference weights, followed by duration of hospitalization and chance of 2-year RFS (Figure A). Post-HSCT patients were willing to accept a less effective treatment if it reduced hospital stay or improved QoL: the benefit of a 2-week reduction in hospitalization per year or an improvement of QoL by 35 on a 0-100 scale each compensated for a 30% reduction in 2-year RFS. For physicians, chance of 2-year RFS was the most important treatment attribute, followed by average QoL and risk of serious infections (Figure B). Physicians valued duration of hospitalization and chance of achieving transfusion independence less when selecting treatments. Responses from physicians suggested that a 2-week reduction in hospitalization per year could compensate for having to bear an additional 5% risk of serious infection or 10% risk of nausea.
Conclusion
Differences in treatment attribute importance for post-HSCT maintenance therapy were observed between patients and physicians. The DCE results highlight the value patients place on treatments that improve their QoL and reduce the duration of hospitalization. Physicians also valued patients’ QoL when making treatment decisions, so informing physicians of patients’ preferences may influence their choices regarding treatments that better meet patients’ needs and improve patients’ treatment satisfaction.
Keyword(s): Quality of life, Treatment


