
Contributions
Abstract: S293
Type: Oral Presentation
Session title: Transfusion medicine
Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is currently one of the worst pandemics ever. ABO blood groups are associated with different risk of viral infections and they could also play a role in COVID-19 disease. In vitro, studies demonstrated how anti-A and B antibodies neutralized the infectious capacity of SARS-CoV-2. Both SARS-CoV-2 and antibodies let a strong competitive inhibition of angiotensin converting enzyme 2 (ACE2). Those biological mechanisms could be associated with the lower risk of severity and mortality in blood group O patients.
Aims
Prospectively perform a cytokine array in plasma samples from COVID-19 patients who were stratified based on their bloody type, in order to describe the inflammatory response and provide a further insight about the possible protective mechanisms elicited by the blood type O.
Methods
Prospective and consecutive study including blood samples from 108 adult patients diagnosed with COVID-19 and admitted to the “Hospital Clínico Universitario” (Valladolid, Spain) between March 24 to April 11, 2020. Percentage distribution of ABO blood type correspond to 54.6%, 9.3%, 3.7% and 32.4% for A, B, AB and O group respectively. Patients were divided into 2 groups: i. Blood type O (n=35); ii. Blood types A/B/AB (n=73). Forty-five Cytokines, Chemokines and Growth Factors were measured in duplicate for each patient using a MAGPIX system (Luminex). Statistical analysis was performed using the R statistical package version 4.0.2.
Results
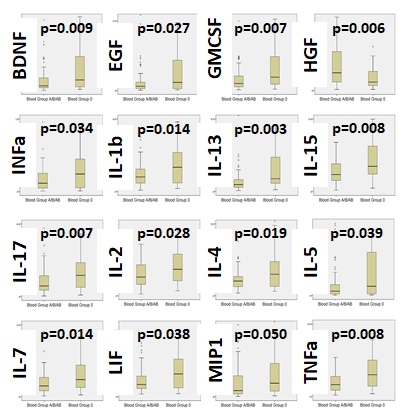
In both groups, most frequent comorbidities were hypertension, diabetes and chronic obstructive pulmonary disease. According to analytical profile, blood type O displayed higher lymphocytes (p=0.057) and lower total bilirubin (p=0.009) plasma levels than the A/B/AB group. We found a lower risk (2.16 times) of mechanical ventilation or death in patients with blood type O [Log Rank: p=0.042, Hazard Ratio: 0.463, CI 95% (0.213-1.004), p=0.050]. Moreover, 15 cytokines were over-express (and 1 under-expressed) in blood type O (Image upload. Left box-plots: Group A/B/AB. Right Box-plots: Group O). Last, a multivariate model found BDNF, IL-13 and IL-27 as the best cytokines able to differentiate the immune profile based on the blood type.
Discussion: In first place, blood type of the general population covered by our hospital are 42%, 9%, 4% and 47% for blood types A, B, AB and O respectively. Nevertheless, our cohort found increase blood type A (54.6%) and decrease in blood type O (32.4%). Therefore, and according our results, blood type O was not only associated to a lower risk of mortality or mechanical ventilation, but also to the need of hospital admission. In second place, a strong ACE2 downregulation – competitive inhibition of ACE2 by SARS-CoV-2 and anti-A and B antibodies – associates high Ang-II plasma levels which allows the production of inflammatory cytokines and, at the same time, a possible lower infectious capacity by SARS-CoV-2 in O blood type patients. Moreover, the existence of a higher activation status of the immune system could also let a rapid activation of the immune response in patients with the O blood type and associate a quicker viral clearance.
Conclusion
Our cohort showed how blood type O associated with both lower rates of hospital admission and lower risk of intubation or death. Indeed, these patients produced higher amounts of cytokines in response to SARS-CoV-2, hence mounting an effective immune response which allowed them to control the viral infection and therefore decrease the risk of further complications.
Keyword(s): ABO blood group, COVID-19, Cytokine, Mortality
Abstract: S293
Type: Oral Presentation
Session title: Transfusion medicine
Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is currently one of the worst pandemics ever. ABO blood groups are associated with different risk of viral infections and they could also play a role in COVID-19 disease. In vitro, studies demonstrated how anti-A and B antibodies neutralized the infectious capacity of SARS-CoV-2. Both SARS-CoV-2 and antibodies let a strong competitive inhibition of angiotensin converting enzyme 2 (ACE2). Those biological mechanisms could be associated with the lower risk of severity and mortality in blood group O patients.
Aims
Prospectively perform a cytokine array in plasma samples from COVID-19 patients who were stratified based on their bloody type, in order to describe the inflammatory response and provide a further insight about the possible protective mechanisms elicited by the blood type O.
Methods
Prospective and consecutive study including blood samples from 108 adult patients diagnosed with COVID-19 and admitted to the “Hospital Clínico Universitario” (Valladolid, Spain) between March 24 to April 11, 2020. Percentage distribution of ABO blood type correspond to 54.6%, 9.3%, 3.7% and 32.4% for A, B, AB and O group respectively. Patients were divided into 2 groups: i. Blood type O (n=35); ii. Blood types A/B/AB (n=73). Forty-five Cytokines, Chemokines and Growth Factors were measured in duplicate for each patient using a MAGPIX system (Luminex). Statistical analysis was performed using the R statistical package version 4.0.2.
Results
In both groups, most frequent comorbidities were hypertension, diabetes and chronic obstructive pulmonary disease. According to analytical profile, blood type O displayed higher lymphocytes (p=0.057) and lower total bilirubin (p=0.009) plasma levels than the A/B/AB group. We found a lower risk (2.16 times) of mechanical ventilation or death in patients with blood type O [Log Rank: p=0.042, Hazard Ratio: 0.463, CI 95% (0.213-1.004), p=0.050]. Moreover, 15 cytokines were over-express (and 1 under-expressed) in blood type O (Image upload. Left box-plots: Group A/B/AB. Right Box-plots: Group O). Last, a multivariate model found BDNF, IL-13 and IL-27 as the best cytokines able to differentiate the immune profile based on the blood type.
Discussion: In first place, blood type of the general population covered by our hospital are 42%, 9%, 4% and 47% for blood types A, B, AB and O respectively. Nevertheless, our cohort found increase blood type A (54.6%) and decrease in blood type O (32.4%). Therefore, and according our results, blood type O was not only associated to a lower risk of mortality or mechanical ventilation, but also to the need of hospital admission. In second place, a strong ACE2 downregulation – competitive inhibition of ACE2 by SARS-CoV-2 and anti-A and B antibodies – associates high Ang-II plasma levels which allows the production of inflammatory cytokines and, at the same time, a possible lower infectious capacity by SARS-CoV-2 in O blood type patients. Moreover, the existence of a higher activation status of the immune system could also let a rapid activation of the immune response in patients with the O blood type and associate a quicker viral clearance.
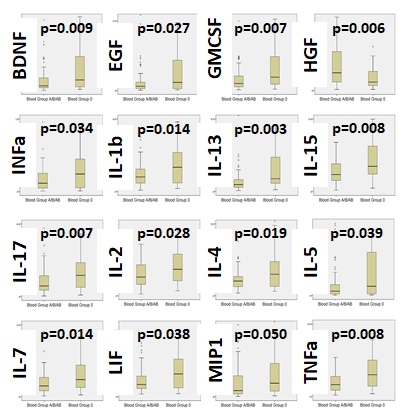
Conclusion
Our cohort showed how blood type O associated with both lower rates of hospital admission and lower risk of intubation or death. Indeed, these patients produced higher amounts of cytokines in response to SARS-CoV-2, hence mounting an effective immune response which allowed them to control the viral infection and therefore decrease the risk of further complications.
Keyword(s): ABO blood group, COVID-19, Cytokine, Mortality


