
Contributions
Abstract: S283
Type: Oral Presentation
Session title: Fungal, bacterial and viral infections in hematology
Background
Invasive fungal lung disease (IFD) is a well-recognised complication post haematopoietic stem-cell transplant (HSCT), occurring in approximately 5-21% of patients, despite tri-azole anti-fungal prophylaxis. Baseline CT thorax (BCT) pre-HSCT is increasingly considered as standard practise to evaluate lung disease, however evidence on outcomes from previous studies has been limited by either small or heterogenous cohorts (Ceesay et al 2018, Bitterman et al 2019).
Aims
A number of smaller heterogenous retrospective studies including our centre's previous study by Ceesay et al, BJH 2018, have been published reporting outcomes and risk factors for IFD associated with abnormal baseline CT chest prior to induction chemnotherapy or transplantation,. Based on these findings, we implemented baseline CT chest in all our high-risk group patients due to undergo allogeneic stem cell transplantation and induction chemotherapies from 2015. Routine biomarkr screening and diagnostic clinical algorithm was implemented. This study then set out to prospectively evaluate utility of baseline CT chest in a homogenous cohort of allo HSCTs and its correlation of different morphological imaging changes and baseline patient related factors associated with risk for IFD.
Methods
We conducted a single centre prospective analysis of patients with myeloid malignancies and aplastic anaemia (n=350) who underwent T-cell deplete allogeneic HSCT between Jan 2015 and April 2019. BCT was performed in 235 (67%) patients within 4 weeks of planned HSCT with biomarker driven IFD screening & diagnostic strategy as standard. IFD was defined as probable/proven disease by European Organisation for Research & Treatment of Cancer(EORTC)-2008 criteria.
Results
Baseline CT was abnormal in 58% of patients (136/235). EORTC defined abnormalities were present in 28% of abnormal CT’s (38/136). Post HSCT, IFD developed in 9.1% of total patients (n=32/350) and in 12.3% (n=29/235) of those who had BCT. Patients with EORTC defined changes on BCT developed more IFD compared to those with normal BCT findings (34.2% vs 9.4%, p=<0.01). Univariate analysis of baseline characteristics identified that a significantly higher proportion of those with history of previous IFD developed post-HSCT IFD (33.3% vs 8.3%; P=<0.01). Reduced intensity conditioning, poor baseline performance status and co-morbidities, and gas transfer (TLCO <70%) significantly influenced the development of IFD. Risk factors for baseline abnormal CT were Age >60 years, higher HCT-CI, pre-existing lung disease and prior history of IFD.
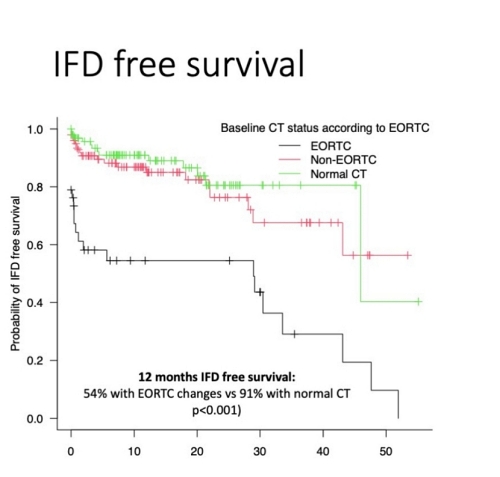
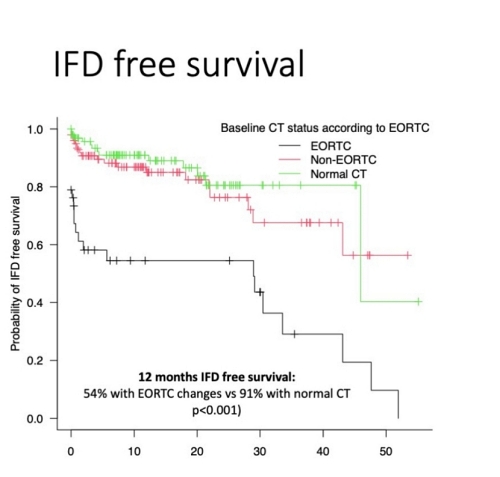
Although presence of abnormal BCT did not influence overall survival, there was a significant reduction in overall survival at 12 months post HSCT in those who developed IFD(62% vs 76%, p=0.001, log rank). Among patients with EORTC defined changes on BCT, there was a significant reduction in median IFD-free survival (30.5 months vs 47 months, p=0.009) when compared to non-EORTC and normal CT findings (see Figure attached). There was a significant reduction in overall survival at 12 months post HSCT in those who developed IFD(62% vs 76%, p=0.001, log rank).
Conclusion
Previous IFD history, EORTC changes & multiple non-EORTC changes at baseline CT and abnormal TLCO pre-HSCT influenced IFD related outcomes with a significant reduction survival post IFD event. We suggest early respiratory optimisation including focussed diagnostics in patients with abnormal pre-HSCT chest imaging, to reduce risk of IFD-related mortality. Further evaluation of impact of interventions in patients with abnormal BCT is warranted.
Keyword(s): Allogeneic hematopoietic stem cell transplant, Invasive pulmonary aspergillosis
Abstract: S283
Type: Oral Presentation
Session title: Fungal, bacterial and viral infections in hematology
Background
Invasive fungal lung disease (IFD) is a well-recognised complication post haematopoietic stem-cell transplant (HSCT), occurring in approximately 5-21% of patients, despite tri-azole anti-fungal prophylaxis. Baseline CT thorax (BCT) pre-HSCT is increasingly considered as standard practise to evaluate lung disease, however evidence on outcomes from previous studies has been limited by either small or heterogenous cohorts (Ceesay et al 2018, Bitterman et al 2019).
Aims
A number of smaller heterogenous retrospective studies including our centre's previous study by Ceesay et al, BJH 2018, have been published reporting outcomes and risk factors for IFD associated with abnormal baseline CT chest prior to induction chemnotherapy or transplantation,. Based on these findings, we implemented baseline CT chest in all our high-risk group patients due to undergo allogeneic stem cell transplantation and induction chemotherapies from 2015. Routine biomarkr screening and diagnostic clinical algorithm was implemented. This study then set out to prospectively evaluate utility of baseline CT chest in a homogenous cohort of allo HSCTs and its correlation of different morphological imaging changes and baseline patient related factors associated with risk for IFD.
Methods
We conducted a single centre prospective analysis of patients with myeloid malignancies and aplastic anaemia (n=350) who underwent T-cell deplete allogeneic HSCT between Jan 2015 and April 2019. BCT was performed in 235 (67%) patients within 4 weeks of planned HSCT with biomarker driven IFD screening & diagnostic strategy as standard. IFD was defined as probable/proven disease by European Organisation for Research & Treatment of Cancer(EORTC)-2008 criteria.
Results
Baseline CT was abnormal in 58% of patients (136/235). EORTC defined abnormalities were present in 28% of abnormal CT’s (38/136). Post HSCT, IFD developed in 9.1% of total patients (n=32/350) and in 12.3% (n=29/235) of those who had BCT. Patients with EORTC defined changes on BCT developed more IFD compared to those with normal BCT findings (34.2% vs 9.4%, p=<0.01). Univariate analysis of baseline characteristics identified that a significantly higher proportion of those with history of previous IFD developed post-HSCT IFD (33.3% vs 8.3%; P=<0.01). Reduced intensity conditioning, poor baseline performance status and co-morbidities, and gas transfer (TLCO <70%) significantly influenced the development of IFD. Risk factors for baseline abnormal CT were Age >60 years, higher HCT-CI, pre-existing lung disease and prior history of IFD.
Although presence of abnormal BCT did not influence overall survival, there was a significant reduction in overall survival at 12 months post HSCT in those who developed IFD(62% vs 76%, p=0.001, log rank). Among patients with EORTC defined changes on BCT, there was a significant reduction in median IFD-free survival (30.5 months vs 47 months, p=0.009) when compared to non-EORTC and normal CT findings (see Figure attached). There was a significant reduction in overall survival at 12 months post HSCT in those who developed IFD(62% vs 76%, p=0.001, log rank).
Conclusion
Previous IFD history, EORTC changes & multiple non-EORTC changes at baseline CT and abnormal TLCO pre-HSCT influenced IFD related outcomes with a significant reduction survival post IFD event. We suggest early respiratory optimisation including focussed diagnostics in patients with abnormal pre-HSCT chest imaging, to reduce risk of IFD-related mortality. Further evaluation of impact of interventions in patients with abnormal BCT is warranted.
Keyword(s): Allogeneic hematopoietic stem cell transplant, Invasive pulmonary aspergillosis


