Contributions
Abstract: S243
Type: Oral Presentation
Session title: Stem cell transplantation - Clinical
Background
The FAB Group originally classified CMML as a form of MDS. In 2001, the World Health Organization reclassified the disease as part of a newly created MDS/MPN overlap entity. Even though characterized by high mortality and relapse rates, allo-HCT remains the only curative treatment for both CMML and MDS.
Aims
In this retrospective registry study, we aimed to identify factors associated with allo-HCT outcomes in CMML, particularly focusing on age, and to compare them with MDS outcomes.
Methods
Patients >18 years old who underwent allo-HCT for CMML or MDS between 2010 and 2018 and who were reported to the EBMT registry were included in the analysis. Transformation to AML was an exclusion criterion. CMML outcomes were compared to those of the MDS population transplanted in the same period. Overall Survival (OS) and Relapse Free Survival (RFS) rates were estimated by Kaplan-Meier methods; relapse incidence (REL) and NRM were analyzed as competing risks. Adjusted (cause specific) hazard ratios (HR) were obtained using Cox proportional hazard models. Age was modeled as a continuous linear variable and using restricted cubic splines.
Results
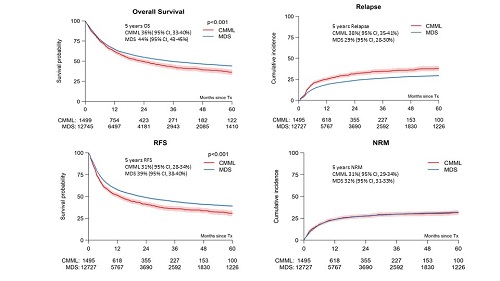
There were 1,499 CMML patients with a median age of 60.4 (18.9-76.3) years and 69.4% were male. 27% had a Karnofsky status ≤80 and 23% of patients had a Sorror HCT-CI ≥3. 28% had HLA-identical sibling donors, 63% unrelated (MUD or MMUD) donors and 8.3% mismatched related donors. A RIC regimen was used in 62%. There were 12,745 MDS patients with a median age of 59.1 (18-79.7) years and 61.1% were male. Regarding Karnofsky scores, Sorror HCT-CI scores, donor types, conditioning regimens and the rates of primary graft failure, there were no clinically meaningful differences between the CMML and MDS groups. OS, RFS and REL rates, were significantly worse in CMML when compared to MDS (all p<0.0001) whereas NRM was not significantly different, p=0.87 (Figure 1). For CMML, the HR for age as a continuous variable at transplantation (adjusted for other confounders), for each 10-year increase of age, was 1.16 (1.06-1.28) for OS and 1.13 (1.04-1.23) for RFS. The HRs for REL and NRM were 1.06 (0.95-1.19) and 1.21 (1.06-1.37) for each 10-year increase in age, respectively. Age≥65 years in the adjusted model conferred a negative impact on OS, RFS and NRM. The same analysis for MDS shows similar results for each 10-year increase of age as those observed for CMML.
Conclusion
The comparison of OS, RFS and REL shows significantly worse outcomes in CMML compared to MDS, with no difference in NRM. As expected, age was associated with poorer outcomes in both diseases. Despite observing these significant differences in survival rates between CMML and MDS, we were not able to identify specific factors other than the diseases themselves. The poorer survival outcomes in CMML in comparison to MDS appear to be the consequence of the significantly higher rate of post-transplant relapse. Future research should focus on post-transplant strategies to improve disease control.
Keyword(s): Chronic myelomonocytic leukemia, Outcome, Stem cell transplant, Survival
Abstract: S243
Type: Oral Presentation
Session title: Stem cell transplantation - Clinical
Background
The FAB Group originally classified CMML as a form of MDS. In 2001, the World Health Organization reclassified the disease as part of a newly created MDS/MPN overlap entity. Even though characterized by high mortality and relapse rates, allo-HCT remains the only curative treatment for both CMML and MDS.
Aims
In this retrospective registry study, we aimed to identify factors associated with allo-HCT outcomes in CMML, particularly focusing on age, and to compare them with MDS outcomes.
Methods
Patients >18 years old who underwent allo-HCT for CMML or MDS between 2010 and 2018 and who were reported to the EBMT registry were included in the analysis. Transformation to AML was an exclusion criterion. CMML outcomes were compared to those of the MDS population transplanted in the same period. Overall Survival (OS) and Relapse Free Survival (RFS) rates were estimated by Kaplan-Meier methods; relapse incidence (REL) and NRM were analyzed as competing risks. Adjusted (cause specific) hazard ratios (HR) were obtained using Cox proportional hazard models. Age was modeled as a continuous linear variable and using restricted cubic splines.
Results
There were 1,499 CMML patients with a median age of 60.4 (18.9-76.3) years and 69.4% were male. 27% had a Karnofsky status ≤80 and 23% of patients had a Sorror HCT-CI ≥3. 28% had HLA-identical sibling donors, 63% unrelated (MUD or MMUD) donors and 8.3% mismatched related donors. A RIC regimen was used in 62%. There were 12,745 MDS patients with a median age of 59.1 (18-79.7) years and 61.1% were male. Regarding Karnofsky scores, Sorror HCT-CI scores, donor types, conditioning regimens and the rates of primary graft failure, there were no clinically meaningful differences between the CMML and MDS groups. OS, RFS and REL rates, were significantly worse in CMML when compared to MDS (all p<0.0001) whereas NRM was not significantly different, p=0.87 (Figure 1). For CMML, the HR for age as a continuous variable at transplantation (adjusted for other confounders), for each 10-year increase of age, was 1.16 (1.06-1.28) for OS and 1.13 (1.04-1.23) for RFS. The HRs for REL and NRM were 1.06 (0.95-1.19) and 1.21 (1.06-1.37) for each 10-year increase in age, respectively. Age≥65 years in the adjusted model conferred a negative impact on OS, RFS and NRM. The same analysis for MDS shows similar results for each 10-year increase of age as those observed for CMML.
Conclusion
The comparison of OS, RFS and REL shows significantly worse outcomes in CMML compared to MDS, with no difference in NRM. As expected, age was associated with poorer outcomes in both diseases. Despite observing these significant differences in survival rates between CMML and MDS, we were not able to identify specific factors other than the diseases themselves. The poorer survival outcomes in CMML in comparison to MDS appear to be the consequence of the significantly higher rate of post-transplant relapse. Future research should focus on post-transplant strategies to improve disease control.
Keyword(s): Chronic myelomonocytic leukemia, Outcome, Stem cell transplant, Survival