
Contributions
Abstract: S240
Type: Oral Presentation
Session title: Stem cell transplantation - Clinical
Background
The use of Tyrosine Kinase Inhibitors (TKIs) post-allogeneic hematopoietic stem cell transplant (post-Allo-SCT) is still heterogeneous and their preventive effect on relapse is not clearly established.
Aims
We performed a sub-analysis, focused on this aspect, of the recent published GITMO study (Candoni et al, BBMT 2019-ClinicalTrials.gov NCT03821727) that included 441 adult patients with Ph-pos ALL, all treated in the induction phase with TKIs± chemotherapy and undergoing Allo-SCT from 2005 to 2017.
Methods
Only cases in morphological complete remission (CcR) before Allo-SCT and receiving a TKI post-Allo-SCT were included in this analysis, regardless of the pre Allo-SCT Minimal Residual Disease (MRD) status (positive or negative). Patients who started TKIs post-Allo-SCT in a condition of cytological relapse were excluded from this study. MRD (BCR-ABL) was monitored monthly for the first 6 months post Allo-SCT and then every 2 months. TKIs were administered after Allo-SCT prophylactically (starting with MRD neg post-Allo-SCT) or pre-emptively (starting at the first MRD positivity post-SCT and without hematological relapse). The attempt of this analysis was to assess the strategy of use of TKIs post-Allo-SCT (prophylactic or pre-emptive) in patients transplanted while in CcR and to verify the probability of survival and leukemia free survival (OS and DFS) post Allo-SCT, based on TKI strategy adopted (prophylactic or pre-emptive) and according to the MRD status pre-Allo-SCT.
Results
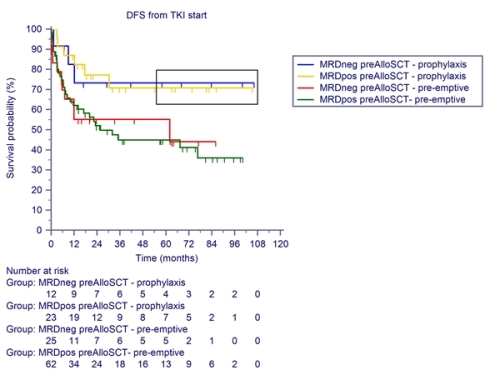
We identified and analyzed 122 cases (85 MRD positive pre-Allo-SCT and 37 MRD negative) that met the inclusion criteria. A pre-emptive TKI strategy was adopted in 87/122-71% cases (25 with MRD neg pre-Allo-SCT) and a prophylactic strategy in 35/122-29% (12 with MRD neg pre-Allo-SCT). The 35 patients treated with TKIs prophylactically started treatment earlier, at a median of 2.97 months (range 0.57-14.17) from Allo-SCT, than the 87 patients treated pre-emptively, which started TKI at a median of 4.37 months (range 0.87-44.27) from Allo-SCT (p=0,01). In the cohort of the MRD pos pre-Allo-SCT, the cases treated pre-emptively had a significant higher percentage of cytological relapse (REL) post-Allo-SCT compared to the cases treated with TKIs prophylactically (cytologic relapse 37% vs 13%, p=0,03). The 5 yrs OS and DFS post Allo-SCT of patients who started TKI in prophylaxis were significantly better (OS 72% and DFS 72%) than those who started TKI in pre-emptive (OS 58% and DFS 47%) regardless of the status of pre-transplant MRD (p=0,008)-FIGURE 1-DFS.
Conclusion
The data obtained from this analysis in a homogeneous population of Ph-pos ALL who underwent Allo-SCT while in CcR, although with the caution of a retrospective study, support the prophylactic use of TKIs post-Allo-SCT as optimal maintenance strategy, resulting in a higher probability of DFS regardless of the MRD status pre-Allo-SCT.
Keyword(s): Acute lymphoblastic leukemia, Allogeneic hematopoietic stem cell transplant, Ph+ ALL, Tyrosine kinase inhibitor
Abstract: S240
Type: Oral Presentation
Session title: Stem cell transplantation - Clinical
Background
The use of Tyrosine Kinase Inhibitors (TKIs) post-allogeneic hematopoietic stem cell transplant (post-Allo-SCT) is still heterogeneous and their preventive effect on relapse is not clearly established.
Aims
We performed a sub-analysis, focused on this aspect, of the recent published GITMO study (Candoni et al, BBMT 2019-ClinicalTrials.gov NCT03821727) that included 441 adult patients with Ph-pos ALL, all treated in the induction phase with TKIs± chemotherapy and undergoing Allo-SCT from 2005 to 2017.
Methods
Only cases in morphological complete remission (CcR) before Allo-SCT and receiving a TKI post-Allo-SCT were included in this analysis, regardless of the pre Allo-SCT Minimal Residual Disease (MRD) status (positive or negative). Patients who started TKIs post-Allo-SCT in a condition of cytological relapse were excluded from this study. MRD (BCR-ABL) was monitored monthly for the first 6 months post Allo-SCT and then every 2 months. TKIs were administered after Allo-SCT prophylactically (starting with MRD neg post-Allo-SCT) or pre-emptively (starting at the first MRD positivity post-SCT and without hematological relapse). The attempt of this analysis was to assess the strategy of use of TKIs post-Allo-SCT (prophylactic or pre-emptive) in patients transplanted while in CcR and to verify the probability of survival and leukemia free survival (OS and DFS) post Allo-SCT, based on TKI strategy adopted (prophylactic or pre-emptive) and according to the MRD status pre-Allo-SCT.
Results
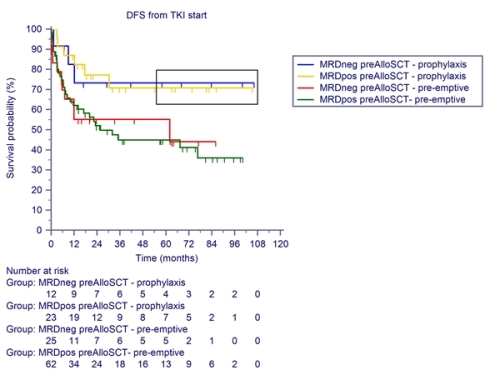
We identified and analyzed 122 cases (85 MRD positive pre-Allo-SCT and 37 MRD negative) that met the inclusion criteria. A pre-emptive TKI strategy was adopted in 87/122-71% cases (25 with MRD neg pre-Allo-SCT) and a prophylactic strategy in 35/122-29% (12 with MRD neg pre-Allo-SCT). The 35 patients treated with TKIs prophylactically started treatment earlier, at a median of 2.97 months (range 0.57-14.17) from Allo-SCT, than the 87 patients treated pre-emptively, which started TKI at a median of 4.37 months (range 0.87-44.27) from Allo-SCT (p=0,01). In the cohort of the MRD pos pre-Allo-SCT, the cases treated pre-emptively had a significant higher percentage of cytological relapse (REL) post-Allo-SCT compared to the cases treated with TKIs prophylactically (cytologic relapse 37% vs 13%, p=0,03). The 5 yrs OS and DFS post Allo-SCT of patients who started TKI in prophylaxis were significantly better (OS 72% and DFS 72%) than those who started TKI in pre-emptive (OS 58% and DFS 47%) regardless of the status of pre-transplant MRD (p=0,008)-FIGURE 1-DFS.
Conclusion
The data obtained from this analysis in a homogeneous population of Ph-pos ALL who underwent Allo-SCT while in CcR, although with the caution of a retrospective study, support the prophylactic use of TKIs post-Allo-SCT as optimal maintenance strategy, resulting in a higher probability of DFS regardless of the MRD status pre-Allo-SCT.
Keyword(s): Acute lymphoblastic leukemia, Allogeneic hematopoietic stem cell transplant, Ph+ ALL, Tyrosine kinase inhibitor


