
Contributions
Abstract: S234
Type: Oral Presentation
Session title: Stem cell transplantation - Preclinical/experimental
Background
Leukemia relapse remains one of the main causes of mortality in acute lymphoblastic leukemia (ALL) patients after allogeneic hematopoietic stem cell transplantation (HSCT). The cumulative incidence of relapse (CIR) was strongly influenced by minimal/measurable residual disease (MRD) assessed at timepoints after or during induction therapy, after consolidation therapy, pre-HSCT and post-HSCT. Besides, other variables, such as the T cell lineage of ALL blasts and remission status after induction therapy or pre-HSCT, have been reported to be correlated with high CIR in those who received allo-HSCT. Consequently, it could be hypothesized that an integrative scoring system mainly based on the quantitative dynamics of MRD in combination with other variables could be more effective in distinguishing ALL cases into different CIR groups.
Aims
The aim of the study was to establish an integrative scoring system, which could provide better relapse risk determination for ALL patients.
Methods
In total, 1416 patients with ALL who underwent HLA-matched sibling donor transplantation (n=285) or haploidentical transplantation (n=1131) were enrolled in this study. A training (retrospective) group (n=651) and a validation (prospective) group (n=765) were included. Factors that were related to CIR were identified in the training group with a multivariate Cox model. A weighted risk score to each factor based on the hazard ratio (HR) from the regression analysis were assigned, and the prognostic score was then defined as the sum of single-risk parameters.
Results
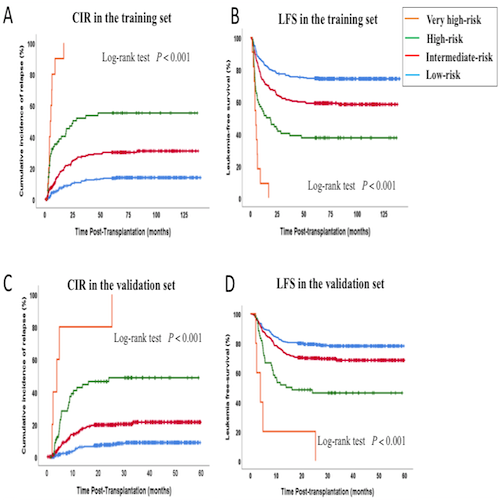
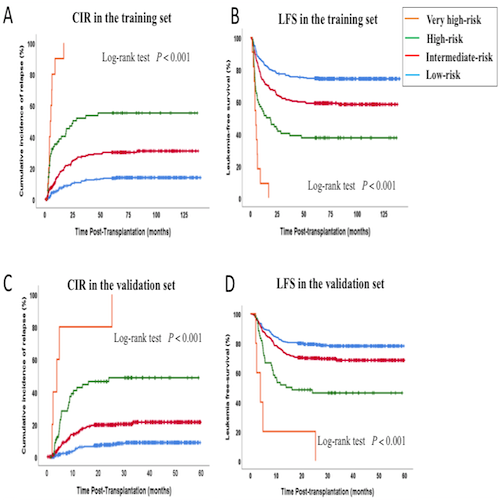
In the training group, four risk groups -- low- (score = 0), intermediate- (score =1-2), high- (score =2.5-6) and very high-risk (score≥6.5) -- were stratified using the scoring system based on remission status before transplantation, immunophenotype, and quantitative dynamics of pretransplant- and posttransplant- minimal residual disease. The 3-year CIRs for the low-, intermediate-, high-, and very high-risk groups were 10.9%, 24.5%, 47.2%, and 90.0%, respectively (P<0.001). The c-statistic of this final model was 0.69. The risk score was confirmed for the 3-year leukemia-free survival (LFS, P<0.001; c=0.62) and overall survival (OS, P<0.001; c=0.63). In the validation group, the 3-year CIRs for the low-, intermediate-, high-, and very high-risk groups were 7.6%, 19.6%, 45.4%, and 100%, respectively (P<0.001, c=0.69). The risk score was confirmed for the 3-year LFS (P<0.001; c=0.59) and OS (P<0.001; c=0.57).
Conclusion
Our data indicate that the integrative scoring system can be used for outcome stratification in ALL patients received allografts.
Keyword(s): ALL, Allogeneic, MRD, Relapse
Abstract: S234
Type: Oral Presentation
Session title: Stem cell transplantation - Preclinical/experimental
Background
Leukemia relapse remains one of the main causes of mortality in acute lymphoblastic leukemia (ALL) patients after allogeneic hematopoietic stem cell transplantation (HSCT). The cumulative incidence of relapse (CIR) was strongly influenced by minimal/measurable residual disease (MRD) assessed at timepoints after or during induction therapy, after consolidation therapy, pre-HSCT and post-HSCT. Besides, other variables, such as the T cell lineage of ALL blasts and remission status after induction therapy or pre-HSCT, have been reported to be correlated with high CIR in those who received allo-HSCT. Consequently, it could be hypothesized that an integrative scoring system mainly based on the quantitative dynamics of MRD in combination with other variables could be more effective in distinguishing ALL cases into different CIR groups.
Aims
The aim of the study was to establish an integrative scoring system, which could provide better relapse risk determination for ALL patients.
Methods
In total, 1416 patients with ALL who underwent HLA-matched sibling donor transplantation (n=285) or haploidentical transplantation (n=1131) were enrolled in this study. A training (retrospective) group (n=651) and a validation (prospective) group (n=765) were included. Factors that were related to CIR were identified in the training group with a multivariate Cox model. A weighted risk score to each factor based on the hazard ratio (HR) from the regression analysis were assigned, and the prognostic score was then defined as the sum of single-risk parameters.
Results
In the training group, four risk groups -- low- (score = 0), intermediate- (score =1-2), high- (score =2.5-6) and very high-risk (score≥6.5) -- were stratified using the scoring system based on remission status before transplantation, immunophenotype, and quantitative dynamics of pretransplant- and posttransplant- minimal residual disease. The 3-year CIRs for the low-, intermediate-, high-, and very high-risk groups were 10.9%, 24.5%, 47.2%, and 90.0%, respectively (P<0.001). The c-statistic of this final model was 0.69. The risk score was confirmed for the 3-year leukemia-free survival (LFS, P<0.001; c=0.62) and overall survival (OS, P<0.001; c=0.63). In the validation group, the 3-year CIRs for the low-, intermediate-, high-, and very high-risk groups were 7.6%, 19.6%, 45.4%, and 100%, respectively (P<0.001, c=0.69). The risk score was confirmed for the 3-year LFS (P<0.001; c=0.59) and OS (P<0.001; c=0.57).
Conclusion
Our data indicate that the integrative scoring system can be used for outcome stratification in ALL patients received allografts.
Keyword(s): ALL, Allogeneic, MRD, Relapse


