
Contributions
Abstract: PB1799
Type: Publication Only
Session title: Stem cell transplantation - Clinical
Background
CNS-GvHD remains a very uncommon entity after allo-HSCT and should be considered in absence of other diseases that justify neurological symptoms. CNS-GvHD criteria were described at Consensus Conference on Clinical Practice in chronic GvHD in 2010.
Aims
To describe a case of CNS-GvHD, a very rare entity still under-reported. We believe all cases should be reported to properly detect and treat this entity.
Methods
A 61-year-old woman diagnosed of mixed phenotype acute myeloid leukemia (AML) in June-20. After chemotherapy, on first remission MRD+, she underwent haploidentical HSCT, after fludarabine and busulfan conditioning; GvHD prophylaxis with cyclophosphamide, cyclosporine A (CsA) and mycophenolate mofetil (MMF). Acute skin GvHD grade IV on day +17, treated with systemic steroids with complete response. On day +59 she was admitted to emergency room with progressive inferior limbs motor deficit and hyperalgesia, followed by confusion, somnolence and visual hallucinations. No fever; adequate adherence to acyclovir, posaconazole and cotrimoxazole prophylaxis. Physical examination: decreased strength in lower limbs, dysesthetic alterations and vivid myotatic reflexes.
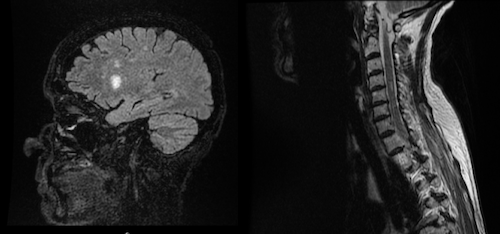
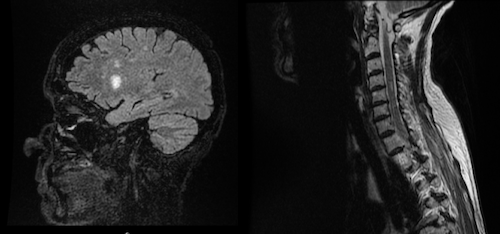
Laboratory findings: no toxic-metabolic abnormalities, normal B12, folic acid and CK levels. Autoimmunity: negative. No schistocytes in blood smear. Nevertheless, CsA was discontinued and MMF started. Cerebrospinal fluid (CSF): no pleocytosis, erythrocytes, nor oligoclonal bands; slight protein elevation (62.1 mg/dL). Microbiological analysis: CMV reactivation in blood sample and positive microarray for HHV-7 in CSF (negative in blood sample). Clinical relevance of HHV-7 was evaluated by neurologists, discarding it as the cause of the picture. Both viruses were covered with foscarnet since admittance, completing 4 weeks treatment. No evidence of EBV, HSV, VZV, HHV-6, HHV-8, polyomavirus, enterovirus, coxackie, toxoplasma, bacterial or fungal infection in CSF. Broad spectrum antibiotics and amphotericin B were also started. AML relapse was ruled out with marrow full donor chimerism and normal immunophenotype in CSF. Electromyography: motor polyneuropathy without demyelination. Cervical spine MRI: hyperintense lesion in T2 at C4-C5 affecting posterior cords; brain MRI: multiple hyperintense lesions in T2 affecting both hemispheres.
During hospitalization she developed gastrointestinal GvHD grade II, so we started methylprednisolone, with partial response. Simultaneously, neurological picture deteriorated with progressively impaired motor function, bradypsychia and dysphagia. New brain MRI showed lesions exacerbation.
Results
Methylprednisolone was substituted for dexamethasone, adding immunoglobulins, with improvement of consciousness, language and dysphagia within 48h; more discreet improvement of motor impairment. Dexamethasone was tapered with sustained neurological effect. A month later, under posaconazole prophylaxis, she developed fungal pneumonia without response to amphotericin B and isavuconazole and died due to respiratory failure.
Conclusion
Neurological complications after allo-HSCT present a wide variety of symptoms, associating high morbi-mortality. Our case exhibits CNS and peripheral nervous symptoms, not classifiable in any entity, with infectious, toxic or vascular etiologies as well as AML relapse discarded. Our patient met mandatory criteria for CNS-GvHD, with neurological worsening concurring in time with exacerbation of intestinal GvHD, and 3 facultative criteria, showing a rapid symptoms improvement after starting dexamethasone, so we assumed it as a neurological manifestation of GvHD.
Keyword(s): Allogeneic hematopoietic stem cell transplant, Graft-versus-host disease (GVHD)
Abstract: PB1799
Type: Publication Only
Session title: Stem cell transplantation - Clinical
Background
CNS-GvHD remains a very uncommon entity after allo-HSCT and should be considered in absence of other diseases that justify neurological symptoms. CNS-GvHD criteria were described at Consensus Conference on Clinical Practice in chronic GvHD in 2010.
Aims
To describe a case of CNS-GvHD, a very rare entity still under-reported. We believe all cases should be reported to properly detect and treat this entity.
Methods
A 61-year-old woman diagnosed of mixed phenotype acute myeloid leukemia (AML) in June-20. After chemotherapy, on first remission MRD+, she underwent haploidentical HSCT, after fludarabine and busulfan conditioning; GvHD prophylaxis with cyclophosphamide, cyclosporine A (CsA) and mycophenolate mofetil (MMF). Acute skin GvHD grade IV on day +17, treated with systemic steroids with complete response. On day +59 she was admitted to emergency room with progressive inferior limbs motor deficit and hyperalgesia, followed by confusion, somnolence and visual hallucinations. No fever; adequate adherence to acyclovir, posaconazole and cotrimoxazole prophylaxis. Physical examination: decreased strength in lower limbs, dysesthetic alterations and vivid myotatic reflexes.
Laboratory findings: no toxic-metabolic abnormalities, normal B12, folic acid and CK levels. Autoimmunity: negative. No schistocytes in blood smear. Nevertheless, CsA was discontinued and MMF started. Cerebrospinal fluid (CSF): no pleocytosis, erythrocytes, nor oligoclonal bands; slight protein elevation (62.1 mg/dL). Microbiological analysis: CMV reactivation in blood sample and positive microarray for HHV-7 in CSF (negative in blood sample). Clinical relevance of HHV-7 was evaluated by neurologists, discarding it as the cause of the picture. Both viruses were covered with foscarnet since admittance, completing 4 weeks treatment. No evidence of EBV, HSV, VZV, HHV-6, HHV-8, polyomavirus, enterovirus, coxackie, toxoplasma, bacterial or fungal infection in CSF. Broad spectrum antibiotics and amphotericin B were also started. AML relapse was ruled out with marrow full donor chimerism and normal immunophenotype in CSF. Electromyography: motor polyneuropathy without demyelination. Cervical spine MRI: hyperintense lesion in T2 at C4-C5 affecting posterior cords; brain MRI: multiple hyperintense lesions in T2 affecting both hemispheres.
During hospitalization she developed gastrointestinal GvHD grade II, so we started methylprednisolone, with partial response. Simultaneously, neurological picture deteriorated with progressively impaired motor function, bradypsychia and dysphagia. New brain MRI showed lesions exacerbation.
Results
Methylprednisolone was substituted for dexamethasone, adding immunoglobulins, with improvement of consciousness, language and dysphagia within 48h; more discreet improvement of motor impairment. Dexamethasone was tapered with sustained neurological effect. A month later, under posaconazole prophylaxis, she developed fungal pneumonia without response to amphotericin B and isavuconazole and died due to respiratory failure.
Conclusion
Neurological complications after allo-HSCT present a wide variety of symptoms, associating high morbi-mortality. Our case exhibits CNS and peripheral nervous symptoms, not classifiable in any entity, with infectious, toxic or vascular etiologies as well as AML relapse discarded. Our patient met mandatory criteria for CNS-GvHD, with neurological worsening concurring in time with exacerbation of intestinal GvHD, and 3 facultative criteria, showing a rapid symptoms improvement after starting dexamethasone, so we assumed it as a neurological manifestation of GvHD.
Keyword(s): Allogeneic hematopoietic stem cell transplant, Graft-versus-host disease (GVHD)


