
Contributions
Abstract: PB1768
Type: Publication Only
Session title: Sickle cell disease
Background
Sickle cell disease (SCD) is an inherited disorder affecting the red blood cells that causes lifelong complications. Vaso-occlusive crises (VOCs), which result from blood vessel obstruction, are clinical hallmarks of SCD. VOCs are associated with intense pain and can lead to potentially irreversible organ damage, and thus can represent a significant clinical burden.
Aims
To assess the risk of VOC by age in patients with SCD using data from a retrospective database analysis.
Methods
The IBM MarketScan Commercial Claims and Medicare Supplemental Claims databases (July 1, 2013 to June 30, 2018) were used for a retrospective analysis of patients with SCD. Patients with ≥2 SCD diagnoses (ICD-9 CM and ICD-10 CM) on separate claims between July 1, 2013 and January 1, 2017, who were ≥6 years of age on January 1, 2017, and had continuous enrollment throughout a 1-year analysis period (January 1, 2017 to December 31, 2017) were included in this analysis. Patients with >100 inpatient or outpatient VOC-related days, as of January 1, 2017, were excluded from the analysis. Patient demographics and clinical characteristics were assessed using descriptive statistics. In addition, the monthly VOC risk by age, proportion of VOCs experienced by clinical setting, and time to second VOC were evaluated.
Results
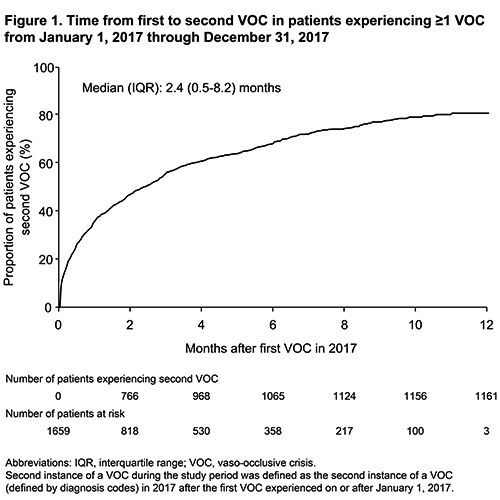
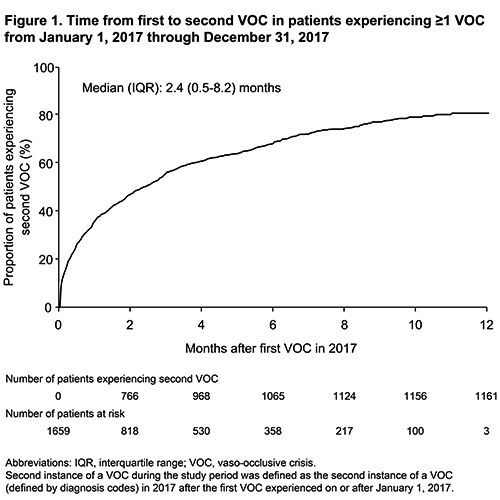
All inclusion criteria were met by 8174 patients. The median (interquartile range) age was 42 (24–55) years and 36.5% of the patients were male. A total of 1659 (20.3%) patients had ≥1 VOC diagnosis during the 1-year study period. The mean (SD) Charlson Comorbidity Index was 0.6 (1.3) and the most common component conditions were chronic pulmonary disease (n=1117 [13.7%]), mild to moderate diabetes (n=608 [7.4%]), renal disease (n=445 [5.4%]), and cerebrovascular disease (n=438 [5.4%]). Patients experienced VOCs in both the outpatient and inpatient setting, and the mean (SD) proportion of VOCs experienced in an outpatient setting was 0.74 (0.34). The mean (SD) monthly VOC risk was 0.07 (0.19). Patients aged ≥20 and <30 years (n=939) had the highest mean (SD) monthly VOC risk (0.16 [0.28]). Among the 1659 patients with ≥1 VOC, 1161 (70.0%) experienced a second VOC during the study period. The time from first to second VOC for all patients with ≥1 VOC within the 1-year study period is shown in Figure 1.
Conclusion
The findings of this study show that patients with SCD often experience recurring VOCs and that younger patients appear to be at greater risk of VOC events.
Keyword(s): Sickle cell disease, Vasoocclusive crisis
Abstract: PB1768
Type: Publication Only
Session title: Sickle cell disease
Background
Sickle cell disease (SCD) is an inherited disorder affecting the red blood cells that causes lifelong complications. Vaso-occlusive crises (VOCs), which result from blood vessel obstruction, are clinical hallmarks of SCD. VOCs are associated with intense pain and can lead to potentially irreversible organ damage, and thus can represent a significant clinical burden.
Aims
To assess the risk of VOC by age in patients with SCD using data from a retrospective database analysis.
Methods
The IBM MarketScan Commercial Claims and Medicare Supplemental Claims databases (July 1, 2013 to June 30, 2018) were used for a retrospective analysis of patients with SCD. Patients with ≥2 SCD diagnoses (ICD-9 CM and ICD-10 CM) on separate claims between July 1, 2013 and January 1, 2017, who were ≥6 years of age on January 1, 2017, and had continuous enrollment throughout a 1-year analysis period (January 1, 2017 to December 31, 2017) were included in this analysis. Patients with >100 inpatient or outpatient VOC-related days, as of January 1, 2017, were excluded from the analysis. Patient demographics and clinical characteristics were assessed using descriptive statistics. In addition, the monthly VOC risk by age, proportion of VOCs experienced by clinical setting, and time to second VOC were evaluated.
Results
All inclusion criteria were met by 8174 patients. The median (interquartile range) age was 42 (24–55) years and 36.5% of the patients were male. A total of 1659 (20.3%) patients had ≥1 VOC diagnosis during the 1-year study period. The mean (SD) Charlson Comorbidity Index was 0.6 (1.3) and the most common component conditions were chronic pulmonary disease (n=1117 [13.7%]), mild to moderate diabetes (n=608 [7.4%]), renal disease (n=445 [5.4%]), and cerebrovascular disease (n=438 [5.4%]). Patients experienced VOCs in both the outpatient and inpatient setting, and the mean (SD) proportion of VOCs experienced in an outpatient setting was 0.74 (0.34). The mean (SD) monthly VOC risk was 0.07 (0.19). Patients aged ≥20 and <30 years (n=939) had the highest mean (SD) monthly VOC risk (0.16 [0.28]). Among the 1659 patients with ≥1 VOC, 1161 (70.0%) experienced a second VOC during the study period. The time from first to second VOC for all patients with ≥1 VOC within the 1-year study period is shown in Figure 1.
Conclusion
The findings of this study show that patients with SCD often experience recurring VOCs and that younger patients appear to be at greater risk of VOC events.
Keyword(s): Sickle cell disease, Vasoocclusive crisis


