
Contributions
Abstract: PB1762
Type: Publication Only
Session title: Sickle cell disease
Background
Sickle cell disease (SCD) is a group of blood disorders with a range of clinical complications, mostly driven by hemolytic anemia and vaso-occlusion. Vaso-occlusive crises (VOCs) are the hallmark of SCD and the most common cause of patient (pt) hospitalization. Despite the potential severe consequences of VOCs, many pts manage them at home. Previous reports from SWAY showed that 24% of pts managed their VOCs at home (not exclusively), primarily because of a poor prior experience in the emergency room (ER)/hospital (Osunkwo I et al. ASH 2019; abstract 2297).
Aims
To assess whether pt-reported impact of SCD on daily life in SWAY differs between pts who reported managing their VOCs exclusively in the ER/hospital vs exclusively at home in the 12 months prior to survey completion.
Methods
SWAY was developed by international SCD experts, pt advocacy groups and Novartis. Pts with SCD aged ≥6 years completed the survey between April and October 2019 (completion by proxy [parent/guardian/caregiver] was required for pts aged 6–11 years, optional for older pts). In SWAY, VOCs were defined as ‘severe pain crises’ and were self-reported by the pt or relevant proxy. Responses to questions on the impact of SCD on daily life were classified on a 1–7 Likert scale (1=not severe/strongly disagree, 7=worst imaginable/strongly agree; 5–7 indicated high impact/agreement).
Results
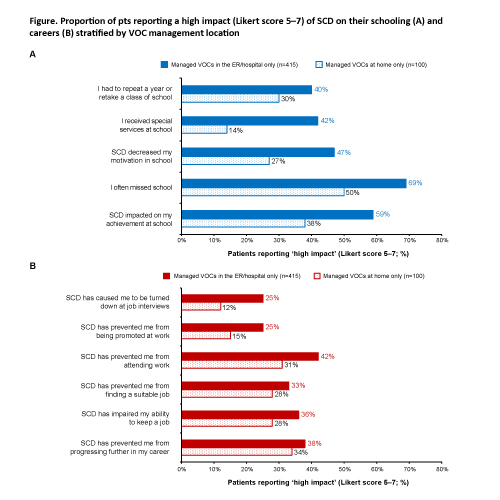
2145 pts from 16 countries across six regions were included in SWAY; 11,317 VOCs were reported in the 12 months prior to survey completion. Of these pts, 29% (n=629) reported managing their VOCs in the ER/hospital (mean age, 24.6 [SD 12.4] years; female, n=331 [53%]; median of 3 [IQR 1–4] VOCs) and 6% (n=134) reported managing VOCs at home (mean age, 27.5 [SD 13.6] years; female, n=71 [53%]; median of 2 [IQR 1–4] VOCs). A greater proportion of pts who reported managing their VOCs in the ER/hospital (n=629) vs at home (n=134) reported a high negative impact of SCD on their emotional wellbeing (61% vs 49%). Of pts managing their VOCs in the ER/hospital, 49%, 45% and 49% rated their level of agreement with the statements ‘I feel stressed’, ‘I feel depressed’ and ‘I worry about dying’, respectively, in the high impact range, compared with 37%, 33% and 36% of pts who managed their VOCs at home. A greater proportion of pts who reported managing their VOCs in the ER/hospital vs at home reported a high impact of SCD on aspects of their daily life, including family/social life (37% vs 27%), relationship with their spouse/partner (33% vs 17%), sexual desire/activity (33% vs 19%) and, to a lesser extent, household daily activities (eg housework, childcare; 32% vs 25%). Self-reported impact of SCD on aspects of schooling and employment also appeared to be higher in pts who managed their VOCs in the ER/hospital vs at home (Figure).
Conclusion
Pts managing their VOCs in the ER/hospital reported a greater impact of SCD on daily life than pts who managed them at home. This may indicate that pts visited the ER/hospital because their pain was too severe to manage at home. Pts experiencing a high impact of SCD on daily life may also seek ER/hospital care for VOCs for psychological support. Equally, visiting the ER/hospital for VOC management may itself be a detriment to pts’ daily lives. Differences in access to healthcare facilities amongst participating countries in SWAY, as well as differing numbers of pts who managed VOCs in the ER/hospital vs at home – possibly influenced by pts’ varied geographic location – may also contribute to the observed differences in this analysis.
Keyword(s): Sickle cell disease, Vasoocclusive crisis
Abstract: PB1762
Type: Publication Only
Session title: Sickle cell disease
Background
Sickle cell disease (SCD) is a group of blood disorders with a range of clinical complications, mostly driven by hemolytic anemia and vaso-occlusion. Vaso-occlusive crises (VOCs) are the hallmark of SCD and the most common cause of patient (pt) hospitalization. Despite the potential severe consequences of VOCs, many pts manage them at home. Previous reports from SWAY showed that 24% of pts managed their VOCs at home (not exclusively), primarily because of a poor prior experience in the emergency room (ER)/hospital (Osunkwo I et al. ASH 2019; abstract 2297).
Aims
To assess whether pt-reported impact of SCD on daily life in SWAY differs between pts who reported managing their VOCs exclusively in the ER/hospital vs exclusively at home in the 12 months prior to survey completion.
Methods
SWAY was developed by international SCD experts, pt advocacy groups and Novartis. Pts with SCD aged ≥6 years completed the survey between April and October 2019 (completion by proxy [parent/guardian/caregiver] was required for pts aged 6–11 years, optional for older pts). In SWAY, VOCs were defined as ‘severe pain crises’ and were self-reported by the pt or relevant proxy. Responses to questions on the impact of SCD on daily life were classified on a 1–7 Likert scale (1=not severe/strongly disagree, 7=worst imaginable/strongly agree; 5–7 indicated high impact/agreement).
Results
2145 pts from 16 countries across six regions were included in SWAY; 11,317 VOCs were reported in the 12 months prior to survey completion. Of these pts, 29% (n=629) reported managing their VOCs in the ER/hospital (mean age, 24.6 [SD 12.4] years; female, n=331 [53%]; median of 3 [IQR 1–4] VOCs) and 6% (n=134) reported managing VOCs at home (mean age, 27.5 [SD 13.6] years; female, n=71 [53%]; median of 2 [IQR 1–4] VOCs). A greater proportion of pts who reported managing their VOCs in the ER/hospital (n=629) vs at home (n=134) reported a high negative impact of SCD on their emotional wellbeing (61% vs 49%). Of pts managing their VOCs in the ER/hospital, 49%, 45% and 49% rated their level of agreement with the statements ‘I feel stressed’, ‘I feel depressed’ and ‘I worry about dying’, respectively, in the high impact range, compared with 37%, 33% and 36% of pts who managed their VOCs at home. A greater proportion of pts who reported managing their VOCs in the ER/hospital vs at home reported a high impact of SCD on aspects of their daily life, including family/social life (37% vs 27%), relationship with their spouse/partner (33% vs 17%), sexual desire/activity (33% vs 19%) and, to a lesser extent, household daily activities (eg housework, childcare; 32% vs 25%). Self-reported impact of SCD on aspects of schooling and employment also appeared to be higher in pts who managed their VOCs in the ER/hospital vs at home (Figure).
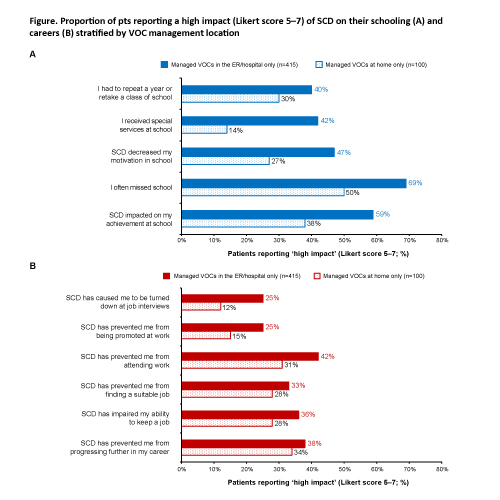
Conclusion
Pts managing their VOCs in the ER/hospital reported a greater impact of SCD on daily life than pts who managed them at home. This may indicate that pts visited the ER/hospital because their pain was too severe to manage at home. Pts experiencing a high impact of SCD on daily life may also seek ER/hospital care for VOCs for psychological support. Equally, visiting the ER/hospital for VOC management may itself be a detriment to pts’ daily lives. Differences in access to healthcare facilities amongst participating countries in SWAY, as well as differing numbers of pts who managed VOCs in the ER/hospital vs at home – possibly influenced by pts’ varied geographic location – may also contribute to the observed differences in this analysis.
Keyword(s): Sickle cell disease, Vasoocclusive crisis


