
Contributions
Abstract: PB1734
Type: Publication Only
Session title: Platelet disorders
Background
Inmune cytopenias (IC) are a frecuent finding that may occur either isolated or associated with autoimmune, neoplasic or infectious diseases. Anemia and thrombocytopenia are the most usual concomitant cytopenias and they even constitute a syndrome (Evans Syndrome-ES) themselves with specific characteristics and prognostic implications. Futhermore, when they are related with another medical condition, the presence of IC may affect unfavorably its treatment and evolution. However, it is not unusual that in some mild onsets this coexistence may be not detected until long time evolution because, for example, haemolytic activity is well-balanced and no anemia or thrombocytopenia are detected or neutropenia is unstable.
Aims
Get a global perspective of the variety of entities with multiple IC that had been referred to Haematology department for assessment and treatment evaluation. Identify those which fulfill classical ES criteria and their treatment and evolution.
Methods
We included 13 adult patients studied between 2006-2020 with autoimmune hemolytic anemia (AIHA) and/or immune thrombocytopenia (ITP) and/or immune neutropenia (IN) in the absence of any underlying cause. A revision of the diagnosis criteria and response to therapy was made according to International Consensus for Adult AIHA and the American Society of Hematology 2019 guidelines for inmune thrombocytopenia. Inmune neutropenia was define by neutrophil count <1,5x10E9/L on at least 2 separate determinations. Finally we defined ES as the concomitant or sequential confirmed presence of 2 of them: AIHA, ITP or IN.
Results
Thirteen patients with confirmed IC were included, 6 males and 7 females with a median age of 42 years at the diagnosis, and a median of 9 years of monitoring. Only 4 patients developed simultaneous cytopenias (2 ITP+IN, 2 ITP+AIHA) and the median of time between one cytopenia and another was 2’5 years. The most frecuent combination found was AIHA+ITP in 12 patients, with lower counts for ITP.
All AIHA were mediated by warm antibodies and antiglobulin test (DAT) IgG1+C3d in 85% of cases with only 1 case IgG+IgA. ITP presentation was moderated to severe in 12 cases. IN was not clinically relevant with a neutrophils nadir over 300x10E9 for all patients, and no recurrent or opportunist infections were documented even though there was 38% cases with significative hipogammaglobulinemia.
Additionally we detected antinuclear positive antibodies in 7 patients, and other types of autoimmune antibodies in 2 patients (antiphospholid and thyroid peroxidase antibodies) with higher titles in those with deeper cytopenias, specially AIHA, and mild to low titles in the rest.
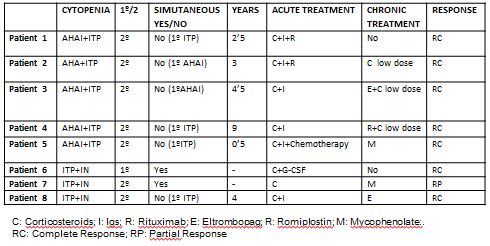
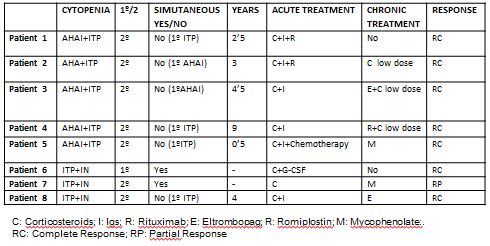
ES criteria were accomplished by 8 patients, 5 AHAI+ITP, 3 ITP+IN. We describe their association with or without an underlying disorder as well as the therapeutic management in Table 1.
Finally, there was not any death related to this autoimmune disorder and 1 patient with secondary ES associated with lung cancer has died for this neoplasic disease.
Conclusion
ES in a rare and probably undiagnosed condition with a treatment traditionally based on corticosteroids. Nowadays combination with TPO-agonists is changing the rules and the prognosis of these patients.
Keyword(s): TPO
Abstract: PB1734
Type: Publication Only
Session title: Platelet disorders
Background
Inmune cytopenias (IC) are a frecuent finding that may occur either isolated or associated with autoimmune, neoplasic or infectious diseases. Anemia and thrombocytopenia are the most usual concomitant cytopenias and they even constitute a syndrome (Evans Syndrome-ES) themselves with specific characteristics and prognostic implications. Futhermore, when they are related with another medical condition, the presence of IC may affect unfavorably its treatment and evolution. However, it is not unusual that in some mild onsets this coexistence may be not detected until long time evolution because, for example, haemolytic activity is well-balanced and no anemia or thrombocytopenia are detected or neutropenia is unstable.
Aims
Get a global perspective of the variety of entities with multiple IC that had been referred to Haematology department for assessment and treatment evaluation. Identify those which fulfill classical ES criteria and their treatment and evolution.
Methods
We included 13 adult patients studied between 2006-2020 with autoimmune hemolytic anemia (AIHA) and/or immune thrombocytopenia (ITP) and/or immune neutropenia (IN) in the absence of any underlying cause. A revision of the diagnosis criteria and response to therapy was made according to International Consensus for Adult AIHA and the American Society of Hematology 2019 guidelines for inmune thrombocytopenia. Inmune neutropenia was define by neutrophil count <1,5x10E9/L on at least 2 separate determinations. Finally we defined ES as the concomitant or sequential confirmed presence of 2 of them: AIHA, ITP or IN.
Results
Thirteen patients with confirmed IC were included, 6 males and 7 females with a median age of 42 years at the diagnosis, and a median of 9 years of monitoring. Only 4 patients developed simultaneous cytopenias (2 ITP+IN, 2 ITP+AIHA) and the median of time between one cytopenia and another was 2’5 years. The most frecuent combination found was AIHA+ITP in 12 patients, with lower counts for ITP.
All AIHA were mediated by warm antibodies and antiglobulin test (DAT) IgG1+C3d in 85% of cases with only 1 case IgG+IgA. ITP presentation was moderated to severe in 12 cases. IN was not clinically relevant with a neutrophils nadir over 300x10E9 for all patients, and no recurrent or opportunist infections were documented even though there was 38% cases with significative hipogammaglobulinemia.
Additionally we detected antinuclear positive antibodies in 7 patients, and other types of autoimmune antibodies in 2 patients (antiphospholid and thyroid peroxidase antibodies) with higher titles in those with deeper cytopenias, specially AIHA, and mild to low titles in the rest.
ES criteria were accomplished by 8 patients, 5 AHAI+ITP, 3 ITP+IN. We describe their association with or without an underlying disorder as well as the therapeutic management in Table 1.
Finally, there was not any death related to this autoimmune disorder and 1 patient with secondary ES associated with lung cancer has died for this neoplasic disease.
Conclusion
ES in a rare and probably undiagnosed condition with a treatment traditionally based on corticosteroids. Nowadays combination with TPO-agonists is changing the rules and the prognosis of these patients.
Keyword(s): TPO


