
Contributions
Abstract: PB1692
Type: Publication Only
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
MM is the 2nd most common hematologic malignancy. It has different overall survival (OS) and progression-free survival (PFS) depending on cytogenetic abnormalities. A 15% of NDMM has an HRC, which supposes an aggressive behaviour, with frequent relapses, until it becomes refractory. There are drugs that partly overcome the adverse effect of HRC on PFS and OS.
Aims
1. Evaluate efficacy and number of relapses until achieving a good treatment response or death. 2. Prognostic impact of clinical-biochemical diagnosis data in a heterogeneous NDMM HRC`s cohort.
Methods
Unicentric, descriptive and retrospective analysis, using clinical and analytical NDMM HRC patient’s data from 2009 to 2020 at Guadalajara University Hospital. HRC is defined by fluorescence in situ hybridization (FISH): mutations on chromosome 1, del17p, t(4;14), t(14;16), t(14;20) or plasmablastic leukemia. Survival data or Cox regression were used. Risk measures; Hazard Ratio (HR) with 95% CI. Negative binomial regression to analyze count variables. P value <0.05 was considered significant.
Results
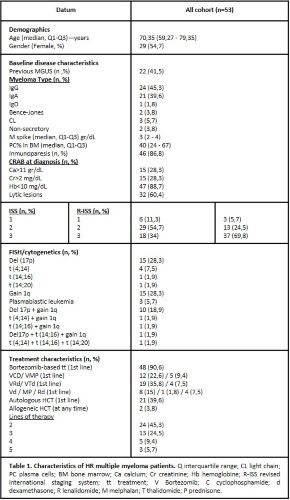
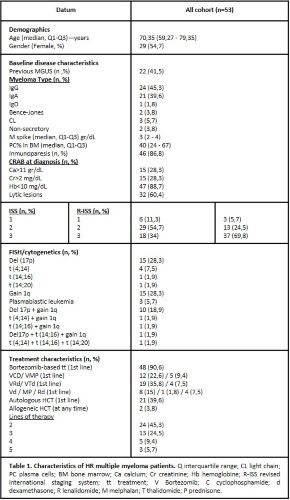
We identified 53 patients (pts) with HRC NDMM, whose clinical characteristics and treatment (tt) data are listed in Table 1. NDMM HRC first-line tt was chosen, regardless of the FISH results: 90,6% of the pts received bortezomib (V) - based induction, of them 35% (n=17) were treated with alkylating agents, 48% (n=23) received immunomodulatory drugs and 17% (n=8) V with dexamethasone (d). Whereas 24,5% (n=13) received a nonintensive tt as Vd, melphalan-d or lenalidomide-d, because they were older than 70 years and the tt was chosen before 2017. Twenty-one pts (39,6%) underwent autologous stem-cell transplantation (ASCT) as part of first-line tt, the vast majority under 65 years. Overall response rate (ORR) after induction was 37%; and declined in subsequent treatment lines, 49% achieved ≥ very good partial response (VGPR).
Median follow-up for surviving patients was 47,25 months (IQ 23,8 – 97, 58). The PFS was 50.26 months (IQ 16.37 - 68.70). 18 pts deceased during the time of the follow-up.
In multivariate analysis to predict OS rate: being a woman (HR: 1.036; p = 0.948) and age >65 years (HR: 1.053; p = 0.087) was associated with a risk factor, but no data showed a statistically significant association.
Equal characteristics such as age, sex, ISS, D&S and analytical data, the only variable that was independently associated with the relapse rate during the follow-up time was ISS-2 versus ISS-1, multiplying by 1,86 the number of times the event appears. Relapse rate: 1.86; p = 0.037) (figure 1).
Conclusion
Our case series presents a longer survival compared to those commented in other studies. It describes similar % cytogenetic abnormalities as in the literature, except for del(17p), which has an incidence of 28.3%. Most frequent combination was the one between 1q gain among pts with del(17p). Our study validates the ISS as the factor with the greatest impact on its prognosis. A longer follow-up and higher HRC NDMM pts`s recruitment will be necessary to better define the response to tt regimens based on individual cytogenetic groups.
Keyword(s): Cytogenetic abnormalities, High risk, Multiple myeloma, Treatment
Abstract: PB1692
Type: Publication Only
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
MM is the 2nd most common hematologic malignancy. It has different overall survival (OS) and progression-free survival (PFS) depending on cytogenetic abnormalities. A 15% of NDMM has an HRC, which supposes an aggressive behaviour, with frequent relapses, until it becomes refractory. There are drugs that partly overcome the adverse effect of HRC on PFS and OS.
Aims
1. Evaluate efficacy and number of relapses until achieving a good treatment response or death. 2. Prognostic impact of clinical-biochemical diagnosis data in a heterogeneous NDMM HRC`s cohort.
Methods
Unicentric, descriptive and retrospective analysis, using clinical and analytical NDMM HRC patient’s data from 2009 to 2020 at Guadalajara University Hospital. HRC is defined by fluorescence in situ hybridization (FISH): mutations on chromosome 1, del17p, t(4;14), t(14;16), t(14;20) or plasmablastic leukemia. Survival data or Cox regression were used. Risk measures; Hazard Ratio (HR) with 95% CI. Negative binomial regression to analyze count variables. P value <0.05 was considered significant.
Results
We identified 53 patients (pts) with HRC NDMM, whose clinical characteristics and treatment (tt) data are listed in Table 1. NDMM HRC first-line tt was chosen, regardless of the FISH results: 90,6% of the pts received bortezomib (V) - based induction, of them 35% (n=17) were treated with alkylating agents, 48% (n=23) received immunomodulatory drugs and 17% (n=8) V with dexamethasone (d). Whereas 24,5% (n=13) received a nonintensive tt as Vd, melphalan-d or lenalidomide-d, because they were older than 70 years and the tt was chosen before 2017. Twenty-one pts (39,6%) underwent autologous stem-cell transplantation (ASCT) as part of first-line tt, the vast majority under 65 years. Overall response rate (ORR) after induction was 37%; and declined in subsequent treatment lines, 49% achieved ≥ very good partial response (VGPR).
Median follow-up for surviving patients was 47,25 months (IQ 23,8 – 97, 58). The PFS was 50.26 months (IQ 16.37 - 68.70). 18 pts deceased during the time of the follow-up.
In multivariate analysis to predict OS rate: being a woman (HR: 1.036; p = 0.948) and age >65 years (HR: 1.053; p = 0.087) was associated with a risk factor, but no data showed a statistically significant association.
Equal characteristics such as age, sex, ISS, D&S and analytical data, the only variable that was independently associated with the relapse rate during the follow-up time was ISS-2 versus ISS-1, multiplying by 1,86 the number of times the event appears. Relapse rate: 1.86; p = 0.037) (figure 1).
Conclusion
Our case series presents a longer survival compared to those commented in other studies. It describes similar % cytogenetic abnormalities as in the literature, except for del(17p), which has an incidence of 28.3%. Most frequent combination was the one between 1q gain among pts with del(17p). Our study validates the ISS as the factor with the greatest impact on its prognosis. A longer follow-up and higher HRC NDMM pts`s recruitment will be necessary to better define the response to tt regimens based on individual cytogenetic groups.
Keyword(s): Cytogenetic abnormalities, High risk, Multiple myeloma, Treatment


