
Contributions
Abstract: PB1675
Type: Publication Only
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
Primary plasma cell leukemia (pPCL) is an infrequent plasma cell disorder that accounts for 1.3%–3.4% of all plasma cell dyscrasias. Its prognosis is poor, with a median survival of 36 months, even after the use of novel drugs. The ideal treatment is not well established. There is scarce data on this disorder in Latin America (LA).
Aims
The aim of this study was to describe demographic, clinical and prognostic characteristics of newly diagnosed pPCL in LA.
Methods
This is a retrospective, multicentric observational study. Patients from 9 countries of LA with diagnosis of pPCL between 2012 and 2020 according to current definition were included. Demographic and clinical data were collected from clinical records. Survival curves were estimated using the Kaplan–Meier method. Uni- and multivariable Cox proportional hazards models were used to assess risk factors.
Results
Sixty patients from Chile, Argentina, Ecuador, Cuba, Perú, México, Paraguay, Colombia and Uruguay were included. Median age was 55 years (range 28 to 92), 53% were male. Anemia was present in 83% at diagnosis (mean 8.1 g/dL), hypercalcemia in 47% (mean 11 mg/dL), renal failure in 50% (mean 2,6 mg/dL of creatinine), thrombocytopenia in 53% (mean 105.000/mm3) bone lytic lesions in 80%. High LDH was observed in 72%. Extramedullary disease was reported in 28% of patients, 3 of them with CNS involvement. Type of paraprotein was IgG in 33%, IgA in 13%, light chain in 45% (55% Kappa), and not reported in 9%. Flow cytometry was performed in 78% of patients, and FISH and conventional cytogenetics in 28%.
Five patients died before receiving any specific treatment. Most patients (83%) were classified as eligible for transplant and received at least 1 cycle of treatment. Thirty-two patients received a bortezomib-based induction, and 17 an intensive chemotherapy-based approach, like VTD-PACE. The most used regimens were CyBorD in 26%, VTD-PACE in 22%, VAD in 16%, and CTD in 14%. Only 1 patient received daratumumab-based therapy. Five patients died during induction, and 12 achieved a complete remission. Twelve patients (24%) received an autologous transplant as consolidation, in 7 cases with tandem modality, and 19% had maintenance therapy. Eleven patients relapsed.
With a median follow up of 16 months, 35 patients (58%) died, and 12 patients remained in complete remission. Median progression free survival (PFS) was 11 months (CI95% 4-18) for the whole cohort, while in patients that receive a bortezomib-based treatment median PFS was 22 months (CI95% 8-73). Median overall survival (OS) was 18 months (CI95% 9-59), and not reached for patients with bortezomib-based induction.
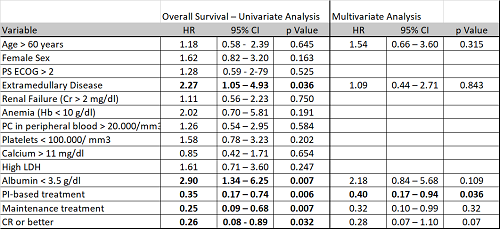
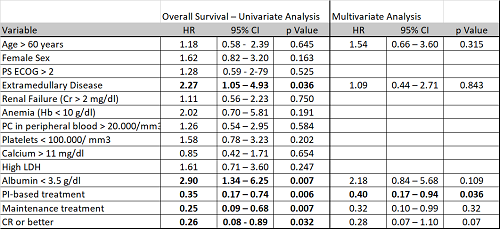
In the multivariate analysis (Table 1) only proteosome inhibitor (PI)-based induction was an independent factor of improved OS.
Conclusion
As reported internationally, LA patients with pPCL were younger than myeloma patients, and clinical features at diagnosis show a more aggressive disease. Of notice, they show more bone lesions than classically described. Reasons for this finding have not been addressed in this analysis. Whether this can be attributed to the use of more sensible imaging techniques or to late diagnosis remain to be elucidated. Frontline therapies were heterogeneous, and autologous transplant were performed in only one quarter of patients. Reasons for 76% of potential candidates not being transplanted merit further analysis. OS is still very poor. Bortezomib-based therapies were associated to improved OS.
Keyword(s): Bortezomib, Myeloma, Plasma cells, Prognostic factor
Abstract: PB1675
Type: Publication Only
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
Primary plasma cell leukemia (pPCL) is an infrequent plasma cell disorder that accounts for 1.3%–3.4% of all plasma cell dyscrasias. Its prognosis is poor, with a median survival of 36 months, even after the use of novel drugs. The ideal treatment is not well established. There is scarce data on this disorder in Latin America (LA).
Aims
The aim of this study was to describe demographic, clinical and prognostic characteristics of newly diagnosed pPCL in LA.
Methods
This is a retrospective, multicentric observational study. Patients from 9 countries of LA with diagnosis of pPCL between 2012 and 2020 according to current definition were included. Demographic and clinical data were collected from clinical records. Survival curves were estimated using the Kaplan–Meier method. Uni- and multivariable Cox proportional hazards models were used to assess risk factors.
Results
Sixty patients from Chile, Argentina, Ecuador, Cuba, Perú, México, Paraguay, Colombia and Uruguay were included. Median age was 55 years (range 28 to 92), 53% were male. Anemia was present in 83% at diagnosis (mean 8.1 g/dL), hypercalcemia in 47% (mean 11 mg/dL), renal failure in 50% (mean 2,6 mg/dL of creatinine), thrombocytopenia in 53% (mean 105.000/mm3) bone lytic lesions in 80%. High LDH was observed in 72%. Extramedullary disease was reported in 28% of patients, 3 of them with CNS involvement. Type of paraprotein was IgG in 33%, IgA in 13%, light chain in 45% (55% Kappa), and not reported in 9%. Flow cytometry was performed in 78% of patients, and FISH and conventional cytogenetics in 28%.
Five patients died before receiving any specific treatment. Most patients (83%) were classified as eligible for transplant and received at least 1 cycle of treatment. Thirty-two patients received a bortezomib-based induction, and 17 an intensive chemotherapy-based approach, like VTD-PACE. The most used regimens were CyBorD in 26%, VTD-PACE in 22%, VAD in 16%, and CTD in 14%. Only 1 patient received daratumumab-based therapy. Five patients died during induction, and 12 achieved a complete remission. Twelve patients (24%) received an autologous transplant as consolidation, in 7 cases with tandem modality, and 19% had maintenance therapy. Eleven patients relapsed.
With a median follow up of 16 months, 35 patients (58%) died, and 12 patients remained in complete remission. Median progression free survival (PFS) was 11 months (CI95% 4-18) for the whole cohort, while in patients that receive a bortezomib-based treatment median PFS was 22 months (CI95% 8-73). Median overall survival (OS) was 18 months (CI95% 9-59), and not reached for patients with bortezomib-based induction.
In the multivariate analysis (Table 1) only proteosome inhibitor (PI)-based induction was an independent factor of improved OS.
Conclusion
As reported internationally, LA patients with pPCL were younger than myeloma patients, and clinical features at diagnosis show a more aggressive disease. Of notice, they show more bone lesions than classically described. Reasons for this finding have not been addressed in this analysis. Whether this can be attributed to the use of more sensible imaging techniques or to late diagnosis remain to be elucidated. Frontline therapies were heterogeneous, and autologous transplant were performed in only one quarter of patients. Reasons for 76% of potential candidates not being transplanted merit further analysis. OS is still very poor. Bortezomib-based therapies were associated to improved OS.
Keyword(s): Bortezomib, Myeloma, Plasma cells, Prognostic factor


